The kidney’s remarkable ability to produce highly concentrated or dilute urine is largely attributed to a sophisticated mechanism known as the countercurrent multiplier system. This article provides a detailed explanation of this system, illustrating how the unique anatomical arrangement of the loop of Henle and collecting ducts creates a steep osmotic gradient in the renal medulla. Understanding the countercurrent multiplier is fundamental to comprehending fluid balance, electrolyte homeostasis, and the pathophysiology of various renal disorders affecting urine concentration.
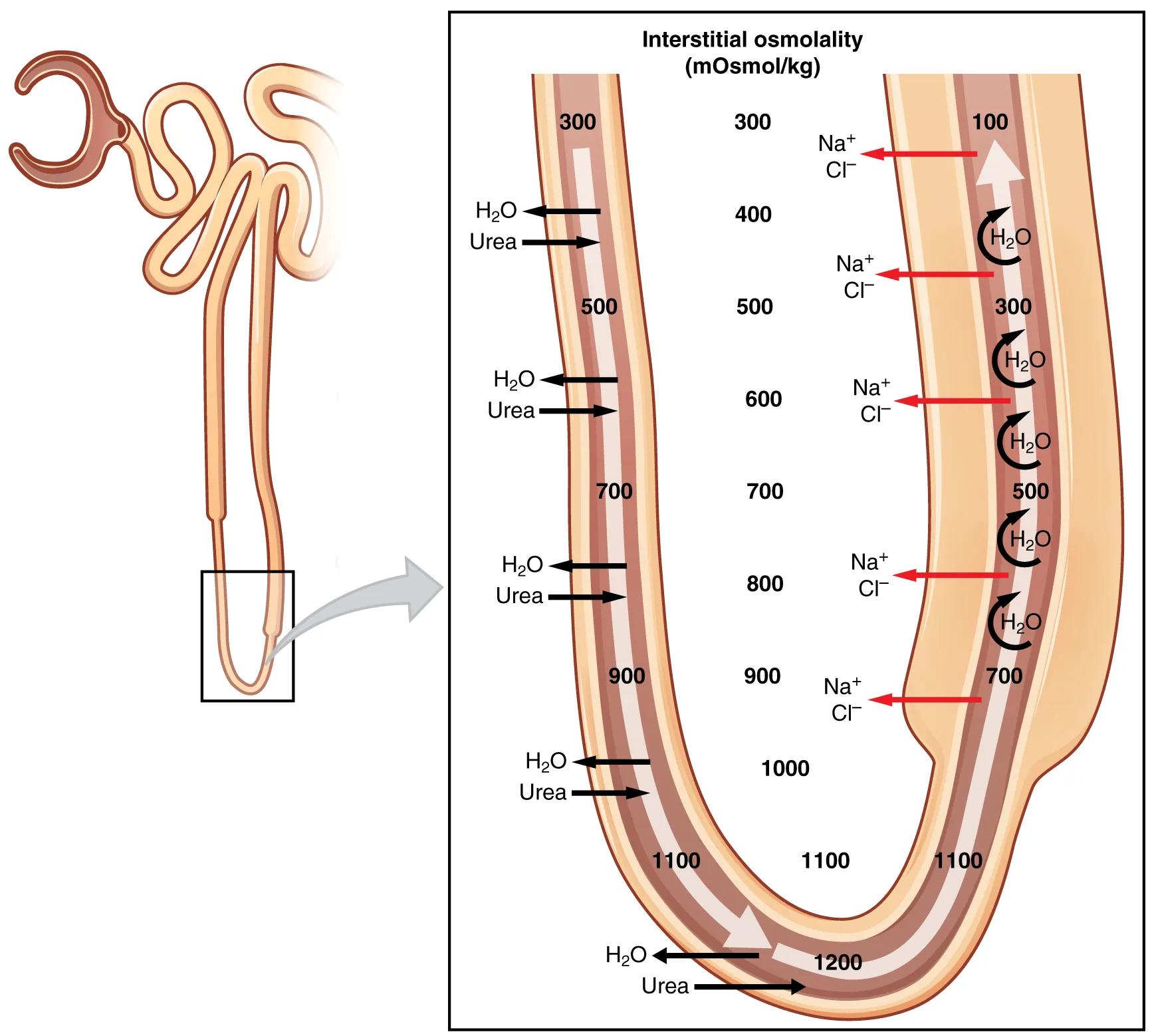
Interstitial osmolality (mOsmol/kg): This refers to the concentration of solutes in the fluid surrounding the renal tubules in the medulla. The countercurrent multiplier system progressively increases this osmolality from the cortex to the deepest part of the medulla, creating a gradient crucial for water reabsorption.
H2O and Urea (black arrows): These indicate the movement of water and urea, primarily out of the descending limb of the loop of Henle and the collecting ducts, driven by the osmotic gradient in the medulla. This reabsorption helps concentrate the urine.
Na+ and Cl- (red arrows): These indicate the active transport of sodium and chloride ions out of the ascending limb of the loop of Henle into the medullary interstitium. This process is crucial for increasing the osmolality of the interstitial fluid.
The human kidney possesses an extraordinary capacity to regulate the body’s water content by producing urine that can be either significantly more concentrated or more dilute than plasma. This precise control is vital for maintaining fluid and electrolyte balance under varying hydration states. The cornerstone of this ability lies in a highly efficient physiological mechanism called the countercurrent multiplier system. This system leverages the unique anatomical configuration of the loops of Henle in juxtamedullary nephrons and their close association with the collecting ducts and vasa recta to establish and maintain a strong osmotic gradient within the renal medulla. This image provides a clear, step-by-step visual explanation of how this intricate system works to concentrate urine.
The countercurrent multiplier system operates through two closely interacting components: the loop of Henle (specifically its descending and ascending limbs) and the collecting ducts, embedded within the gradually increasing interstitial osmolality of the renal medulla. The key principle involves fluid flowing in opposite directions in adjacent segments of the loop, coupled with differential permeabilities to water and solutes.
- Descending Limb: This segment is highly permeable to water but relatively impermeable to solutes. As filtrate descends into the increasingly hypertonic medulla, water passively exits the tubule, concentrating the filtrate within.
- Ascending Limb: This segment is impermeable to water but actively transports sodium (Na+) and chloride (Cl-) ions out of the tubule into the medullary interstitium. This active transport of salts is the “multiplication” step, which progressively increases the osmolality of the interstitial fluid, particularly at the deeper parts of the medulla.
The active pumping of salts by the ascending limb continually adds solutes to the medullary interstitium, while the passive movement of water out of the descending limb helps to concentrate the fluid within it, perpetuating and amplifying the osmotic gradient. This gradient, ranging from approximately 300 mOsmol/kg in the outer cortex to 1200 mOsmol/kg in the inner medulla, is then utilized by the collecting ducts. The collecting ducts are permeable to water, particularly under the influence of antidiuretic hormone (ADH), which causes water to move out of the duct into the hypertonic medullary interstitium, driven by the osmotic gradient created by the loop of Henle. This reabsorption of water, along with some urea, significantly concentrates the final urine.
Dysfunction of the countercurrent multiplier system can lead to severe imbalances in fluid and electrolyte homeostasis. Conditions that impair the ability of the loop of Henle to establish the medullary osmotic gradient, such as damage to the loops themselves or reduced active transport of salts, can result in the inability to produce concentrated urine. This can manifest as nephrogenic diabetes insipidus, where the kidneys cannot respond to ADH, or central diabetes insipidus, where ADH production is deficient. Both lead to excessive urine output (polyuria) and dehydration. Diuretics, particularly loop diuretics, target the ascending limb of the loop of Henle, inhibiting Na+, K+, and Cl- reabsorption, thereby disrupting the countercurrent multiplier and promoting robust diuresis. Understanding this complex physiological mechanism is therefore critical for diagnosing, treating, and managing a wide array of renal and metabolic disorders, ensuring the body’s fluid balance is maintained.

