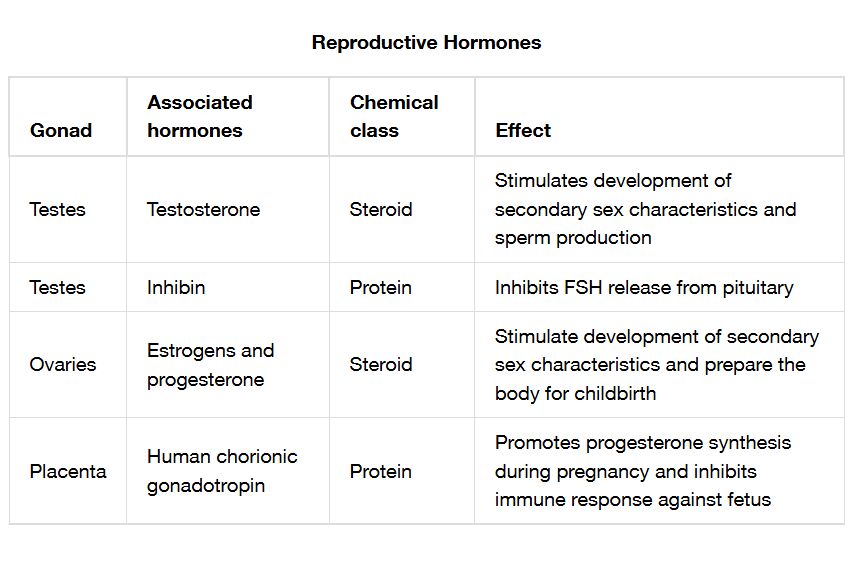
The reproductive system relies on a complex interplay of hormones to regulate fertility, sexual development, and reproductive cycles in both males and females. This article explores a detailed chart of reproductive hormones, their sources, and their physiological effects, providing a comprehensive overview of their roles in maintaining reproductive health.
Hypothalamus The hypothalamus initiates reproductive hormone cascades by releasing gonadotropin-releasing hormone (GnRH). It serves as the control center, responding to internal and external cues to regulate the pituitary gland.
Anterior pituitary The anterior pituitary secretes follicle-stimulating hormone (FSH) and luteinizing hormone (LH) in response to GnRH. These hormones are essential for stimulating gonadal function in both sexes.
Ovaries The ovaries produce estrogen and progesterone in females, driving the menstrual cycle and supporting pregnancy. They also house developing eggs, influenced by pituitary hormones.
Testes The testes produce testosterone in males, promoting sperm production and secondary sexual characteristics. This hormone is regulated by LH and FSH from the pituitary.
Gonadotropin-releasing hormone (GnRH) Gonadotropin-releasing hormone (GnRH) stimulates the anterior pituitary to release FSH and LH. Its pulsatile release ensures proper timing of reproductive events.
Follicle-stimulating hormone (FSH) Follicle-stimulating hormone (FSH) promotes follicle development in females and spermatogenesis in males. It works in concert with LH to support reproductive cell maturation.
Luteinizing hormone (LH) Luteinizing hormone (LH) triggers ovulation in females and testosterone production in males. Its surge is critical for reproductive cycle progression and fertility.
Estrogen Estrogen regulates the menstrual cycle, supports uterine growth, and develops secondary sexual characteristics in females. It is produced primarily by ovarian follicles.
Progesterone Progesterone prepares the uterus for pregnancy and maintains it during gestation. It is secreted by the corpus luteum after ovulation.
Testosterone Testosterone drives sperm production, muscle growth, and male secondary sexual characteristics. It is synthesized in the Leydig cells of the testes.
Inhibin Inhibin, produced by the gonads, inhibits FSH secretion to prevent overproduction of reproductive cells. This feedback mechanism helps regulate the reproductive axis.
Effects Effects of reproductive hormones include sexual development, gamete production, and cycle regulation. These outcomes vary by sex and hormonal balance.
Anatomical Sources of Reproductive Hormones
The reproductive hormone system involves multiple organs working in harmony. This coordination ensures effective regulation of reproductive processes.
- The hypothalamus acts as the initial trigger, releasing GnRH to start the cycle.
- The anterior pituitary responds by secreting FSH and LH.
- Ovaries in females produce estrogen and progesterone for cycle control.
- Testes in males synthesize testosterone for reproductive and physical development.
- Inhibin from the gonads provides negative feedback to the pituitary.
- This anatomical network supports both male and female reproductive health.
Hormone Release and Regulation Mechanisms
The release of reproductive hormones is tightly controlled by feedback loops. This regulation maintains balance and timing in reproductive functions.
- GnRH pulses from the hypothalamus stimulate FSH and LH release.
- FSH supports follicle growth in females and spermatogenesis in males.
- LH triggers ovulation and testosterone production at specific intervals.
- Estrogen and progesterone levels rise and fall with the menstrual cycle.
- Inhibin feedback reduces FSH when gamete production is sufficient.
- This dynamic system prevents hormonal excess or deficiency.
Physiological Effects on Reproductive Health
Reproductive hormones exert specific effects on the body and reproductive organs. Their actions are essential for development and fertility.
- Estrogen promotes breast development and uterine lining growth.
- Progesterone maintains pregnancy by supporting the endometrium.
- Testosterone enhances muscle mass and facial hair growth in males.
- FSH and LH drive egg and sperm maturation, ensuring fertility.
- Inhibin helps fine-tune the reproductive cycle by modulating FSH.
- These effects support sexual maturity and reproductive success.
Clinical Relevance and Associated Disorders
Understanding reproductive hormones aids in diagnosing and treating related conditions. Hormonal imbalances can lead to significant health issues.
- Low GnRH can cause delayed puberty or hypogonadism.
- Excess LH may indicate polycystic ovary syndrome (PCOS), with irregular cycles.
- Reduced testosterone levels lead to low libido or infertility in males.
- High estrogen without progesterone balance can cause endometrial hyperplasia.
- Blood tests measure hormone levels to guide treatments like hormone therapy.
The intricate network of reproductive hormones, originating from the hypothalamus, pituitary, ovaries, and testes, governs sexual development and fertility with precision. The coordinated actions of GnRH, FSH, LH, estrogen, progesterone, testosterone, and inhibin ensure reproductive health, while disorders like PCOS highlight the importance of this system. This knowledge provides a solid foundation for exploring endocrine regulation and clinical interventions.

