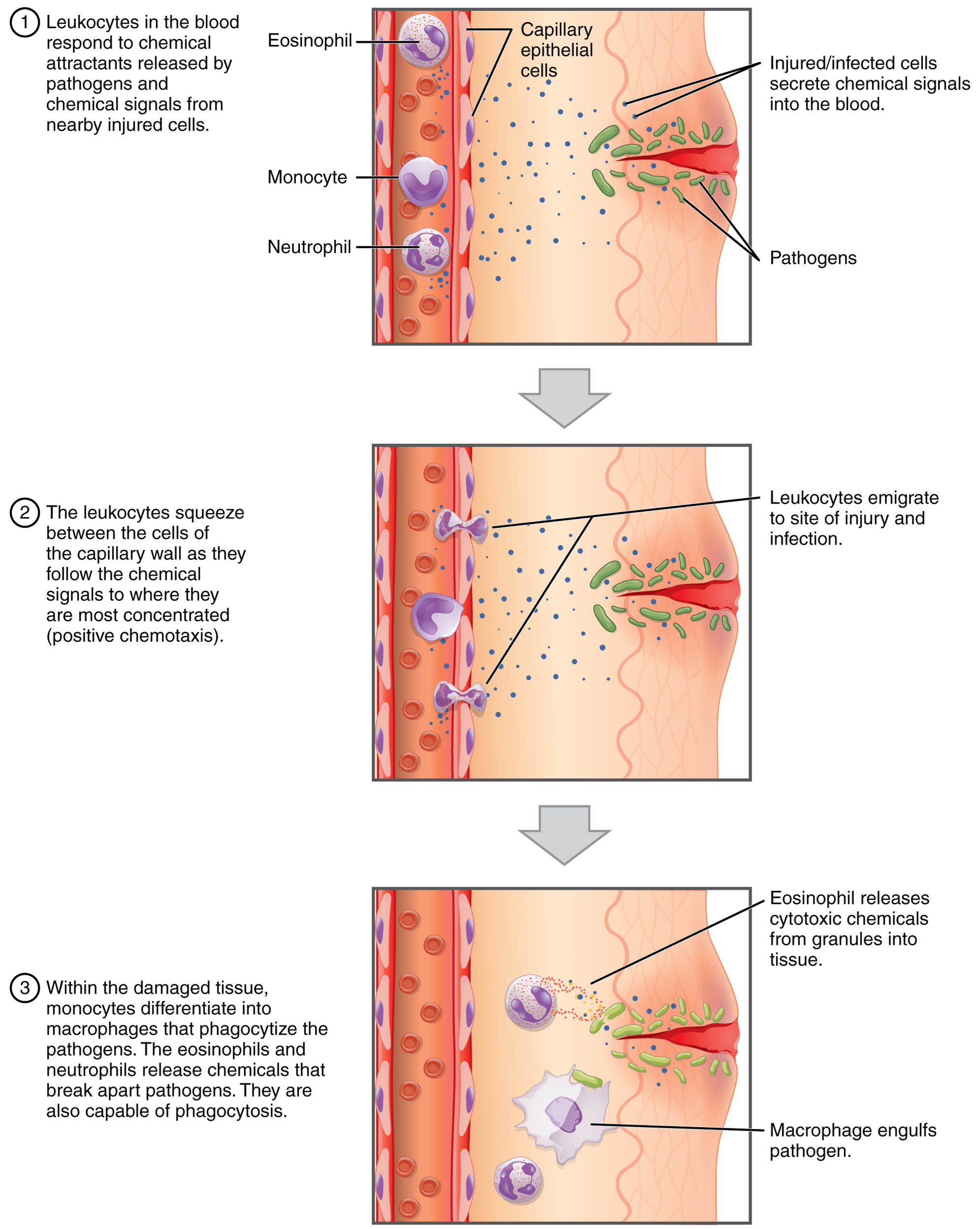
Leukocytes, or white blood cells, are the body’s primary defenders against infection and injury, moving from the bloodstream to sites of inflammation through a process known as emigration. This diagram illustrates the step-by-step journey of leukocytes as they exit capillaries to combat pathogens, highlighting the intricate interactions with endothelial cells and surrounding tissues. Understanding this process sheds light on the immune system’s rapid response to threats and its role in maintaining health.
Key Components of Leukocyte Emigration
The diagram outlines the stages and structures involved in leukocyte movement.
Bloodstream:
The bloodstream serves as the initial transport medium for leukocytes, carrying them through the circulatory system to areas of need. It provides a dynamic environment where leukocytes can respond to chemical signals indicating infection or injury.
Capillary wall:
The capillary wall, composed of endothelial cells, acts as a semi-permeable barrier that leukocytes must cross during emigration. These cells express adhesion molecules that facilitate leukocyte attachment and passage into tissues.
Endothelial cells:
Endothelial cells line the capillary wall and play a key role in regulating leukocyte emigration by expressing selectins and integrins. They respond to inflammatory signals, altering their surface to support leukocyte adhesion and diapedesis.
Selectins:
Selectins are adhesion molecules on endothelial cells that initiate leukocyte rolling by binding to carbohydrate ligands, slowing their movement in the bloodstream. This transient interaction is the first step in the emigration process.
Integrins:
Integrins are adhesion molecules on leukocytes that strengthen binding to endothelial cells after initial rolling, promoting firm adhesion. They are activated by chemokines, enabling leukocytes to prepare for migration.
Chemokines:
Chemokines are signaling proteins released by inflamed tissues that attract leukocytes and activate integrins, guiding their movement. They create a concentration gradient that directs leukocytes to the site of infection or injury.
Leukocyte:
The leukocyte, a white blood cell, undergoes emigration to exit the bloodstream and enter tissues, equipped with receptors for selectins and integrins. Its ability to adapt and respond to inflammatory cues is critical for immune defense.
Rolling:
Rolling is the initial phase where leukocytes slow down along the capillary wall due to selectin-mediated interactions, preparing for further adhesion. This step allows leukocytes to scan for chemokine signals.
Adhesion:
Adhesion involves the firm attachment of leukocytes to endothelial cells via integrins, halting their movement in the bloodstream. This stable binding sets the stage for the leukocyte to migrate through the vessel wall.
Diapedesis:
Diapedesis is the process where leukocytes squeeze between endothelial cells to enter the surrounding tissue, guided by chemokine gradients. This movement is facilitated by cytoskeletal changes within the leukocyte.
Interstitial fluid:
Interstitial fluid surrounds tissues and serves as the medium where emigrated leukocytes travel to reach infection sites. It provides a pathway enriched with nutrients and signaling molecules.
Infected/damaged tissue:
Infected or damaged tissue releases inflammatory mediators that attract leukocytes, marking the destination of their emigration. This area requires immune intervention to resolve infection or repair injury.
The Anatomical and Physiological Role of Leukocyte Emigration
Leukocyte emigration is a cornerstone of the immune response, enabling white blood cells to leave the bloodstream and reach infected/damaged tissue. The process begins with leukocytes interacting with the capillary wall, where endothelial cells upregulate selectins in response to inflammation, initiating rolling. This transient binding allows leukocytes to detect chemokines, which activate integrins for adhesion, anchoring them firmly to the endothelium.
The final step, diapedesis, involves leukocytes passing through the endothelial layer into interstitial fluid, guided by chemokine gradients toward the site of injury. This movement is driven by cytoskeletal reorganization and is critical for phagocytosis and pathogen destruction. Hormones like cortisol can modulate this process, reducing emigration during stress, while thyroid hormones (T3 and T4) influence overall metabolic demand affecting immune activity.
- Adhesion Dynamics: Selectins mediate weak, reversible bonds; integrins form strong, long-lasting attachments.
- Chemokine Function: CXCL8 attracts neutrophils; CCL2 recruits monocytes to chronic inflammation.
- Tissue Penetration: Diapedesis requires PECAM-1 expression on both leukocytes and endothelial cells.
Physical Characteristics and Clinical Relevance
The physical process of leukocyte emigration involves distinct morphological changes, observable under microscopy. During rolling, leukocytes appear to tumble along the endothelium, while adhesion flattens them against the capillary wall. Diapedesis reveals a pseudopodial extension as leukocytes squeeze through intercellular junctions.
Clinically, this diagram aids in understanding immune-related disorders. Impaired emigration, as seen in leukocyte adhesion deficiency (LAD), results from integrin defects, leading to recurrent infections. Elevated emigration markers, like increased neutrophil counts in sepsis, guide antibiotic therapy. Diagnostic tools, including flow cytometry for adhesion molecule expression, and treatments like G-CSF to boost leukocyte production, rely on this process.
- Diagnostic Techniques: Blood smears assess leukocyte morphology; ELISA measures chemokine levels.
- Therapeutic Approaches: Corticosteroids reduce excessive emigration in autoimmune diseases; stem cell transplants correct LAD.
Conclusion
The leukocyte emigration diagram provides a clear roadmap of how white blood cells mobilize to protect the body, from their journey through the bloodstream to their targeted action in infected tissues. This process exemplifies the immune system’s precision and adaptability, ensuring rapid response to pathogens and injury. By mastering these stages, one can better appreciate the diagnostic and therapeutic strategies that support immune health, highlighting the critical role of leukocyte movement in maintaining physiological balance.

