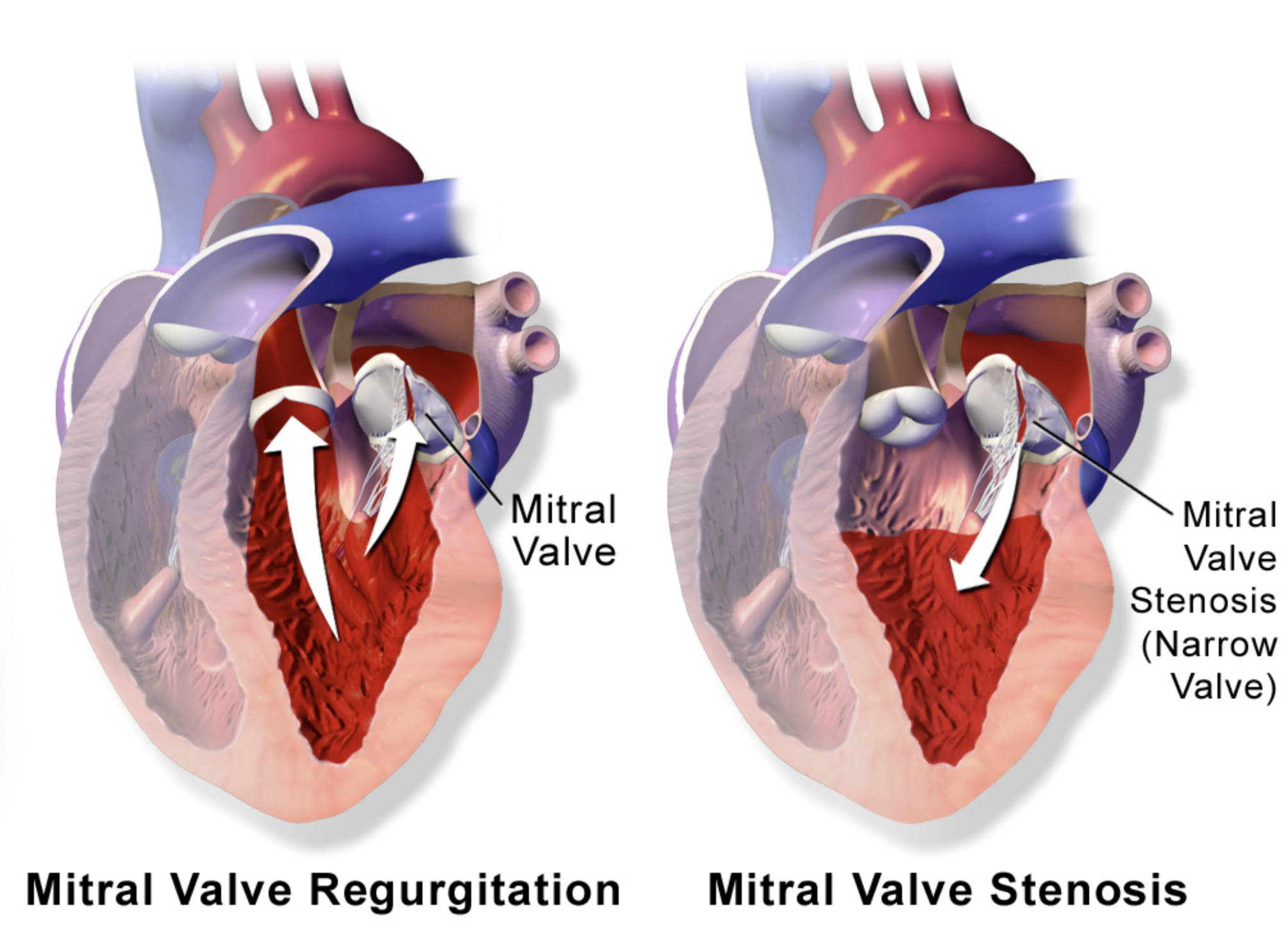
This article explores the critical differences between mitral valve regurgitation and mitral valve stenosis, two common forms of valvular heart disease, as clearly depicted in the provided diagram. We will define each condition, explain their underlying mechanisms, and discuss their impact on cardiac function, offering a comprehensive overview for medical professionals and individuals seeking to understand these important cardiac pathologies.
Mitral Valve: This valve is located between the left atrium and the left ventricle of the heart, playing a crucial role in directing blood flow. Its proper function ensures that blood moves forward from the left atrium into the left ventricle and prevents backflow during ventricular contraction.
Mitral Valve Stenosis (Narrow Valve): This label indicates a condition where the mitral valve opening becomes narrowed, restricting blood flow from the left atrium to the left ventricle. This narrowing forces the heart to work harder to pump blood, often leading to increased pressure in the left atrium.
Mitral Valve Regurgitation: This condition occurs when the mitral valve fails to close properly, allowing blood to leak backward from the left ventricle into the left atrium during ventricular contraction. The diagram illustrates this backflow with an upward arrow, signifying inefficient blood movement.
The mitral valve is a vital component of the heart’s circulatory system, ensuring efficient, one-way blood flow from the left atrium to the left ventricle. When this valve malfunctions, it can lead to significant cardiac issues, broadly categorized into mitral valve regurgitation and mitral valve stenosis. These conditions represent two distinct problems with the valve’s ability to either open fully or close completely, each carrying unique physiological consequences for the heart and the entire circulatory system. The diagram vividly contrasts these two pathologies, highlighting the altered blood flow patterns in each case.
Mitral valve disease can result from a variety of causes, including congenital defects, infections like rheumatic fever, degenerative changes, and ischemic heart disease. Understanding the specific type of mitral valve dysfunction is crucial for accurate diagnosis and effective management. Both conditions place abnormal stress on the heart, but they do so through different mechanisms:
- Mitral valve regurgitation involves a leaky valve, leading to a volume overload in the left atrium and ventricle.
- Mitral valve stenosis involves a narrowed valve, causing a pressure overload in the left atrium.
These distinct hemodynamic changes ultimately influence the heart’s ability to pump blood efficiently to the rest of the body, leading to various symptoms and potential complications.
Mitral Valve Regurgitation: The Leaky Valve
Mitral valve regurgitation (MR) occurs when the mitral valve leaflets do not close tightly during left ventricular systole (contraction), allowing a portion of the blood to flow backward into the left atrium instead of moving forward into the aorta. This backward flow, depicted by the upward arrow in the diagram, is known as regurgitant flow. Over time, the left atrium and left ventricle must work harder to compensate for this inefficiency, leading to their enlargement and increased pressure within the left atrium. The common causes of MR include: mitral valve prolapse, where the valve leaflets bulge into the left atrium during contraction; damage to the chordae tendineae, which are the fibrous cords supporting the valve; rheumatic heart disease; and ischemic heart disease, where a heart attack can damage the papillary muscles that control valve closure.
Symptoms of MR often develop gradually and may include shortness of breath, fatigue, palpitations, and swelling in the legs. In severe cases, MR can lead to heart failure due to the chronic volume overload. The increased workload on the left ventricle can eventually cause it to dilate and weaken, reducing its pumping efficiency. The backflow of blood into the left atrium also raises pressure in the pulmonary circulation, potentially leading to pulmonary hypertension and associated respiratory symptoms. Diagnosis of MR typically involves a physical examination, where a characteristic heart murmur can be heard, followed by an echocardiogram, which provides detailed images of the valve structure and blood flow dynamics. The echocardiogram can accurately assess the severity of the regurgitation and its impact on cardiac chambers.
Mitral Valve Stenosis: The Narrowed Opening
Mitral valve stenosis (MS) is characterized by a narrowing of the mitral valve opening, which obstructs blood flow from the left atrium to the left ventricle during diastole (filling phase). The diagram illustrates this constriction, showing a reduced opening for blood to pass through. This narrowing primarily results from the thickening and fusion of the valve leaflets, often caused by rheumatic fever, which can scar the valve over decades. Less common causes include congenital malformations or calcification. As a result of the obstruction, pressure builds up in the left atrium, causing it to enlarge and potentially leading to the development of atrial fibrillation, an irregular heart rhythm.
The increased pressure in the left atrium is transmitted backward into the pulmonary veins and capillaries, leading to pulmonary congestion and symptoms such as shortness of breath, especially during exertion or when lying flat (orthopnea). Patients with MS may also experience fatigue, chest pain, and recurrent respiratory infections. The chronic elevation of pulmonary pressure can eventually lead to pulmonary hypertension and right heart failure. Diagnosing MS involves listening for a characteristic diastolic murmur during a physical examination, and confirming the diagnosis with an echocardiogram. The echocardiogram allows for precise measurement of the valve opening area, assessment of pressure gradients across the valve, and evaluation of the size and function of the cardiac chambers.
Management and Treatment Approaches
The management of mitral valve disease depends on the severity of the condition, the presence of symptoms, and the patient’s overall health. For mild cases of both regurgitation and stenosis, close monitoring and lifestyle modifications may be sufficient. Medications can help manage symptoms and prevent complications; for instance, diuretics can reduce fluid buildup, and anticoagulants may be prescribed for patients with atrial fibrillation to prevent blood clots. However, when symptoms become severe or heart function is significantly impaired, surgical intervention or transcatheter procedures may be necessary.
For mitral valve regurgitation, repair (mitral valvuloplasty) is often preferred over replacement, as it preserves the patient’s own valve tissue. If repair is not feasible, valve replacement with either a mechanical or bioprosthetic valve is performed. For mitral valve stenosis, balloon valvuloplasty is a minimally invasive procedure that can open the narrowed valve. If this is not suitable, surgical valve replacement or open surgical commissurotomy (repairing the fused leaflets) may be considered. Regular follow-up with a cardiologist is essential for individuals with mitral valve disease to monitor progression and adjust treatment strategies as needed.

