Capillary exchange is a fundamental process in the circulatory system, facilitating the movement of fluids, nutrients, and waste between blood and tissues. This diagram illustrates how net filtration pressure, net reabsorption pressure, and the balance of pressures drive fluid dynamics across the capillary length, from the arterial to the venous end.
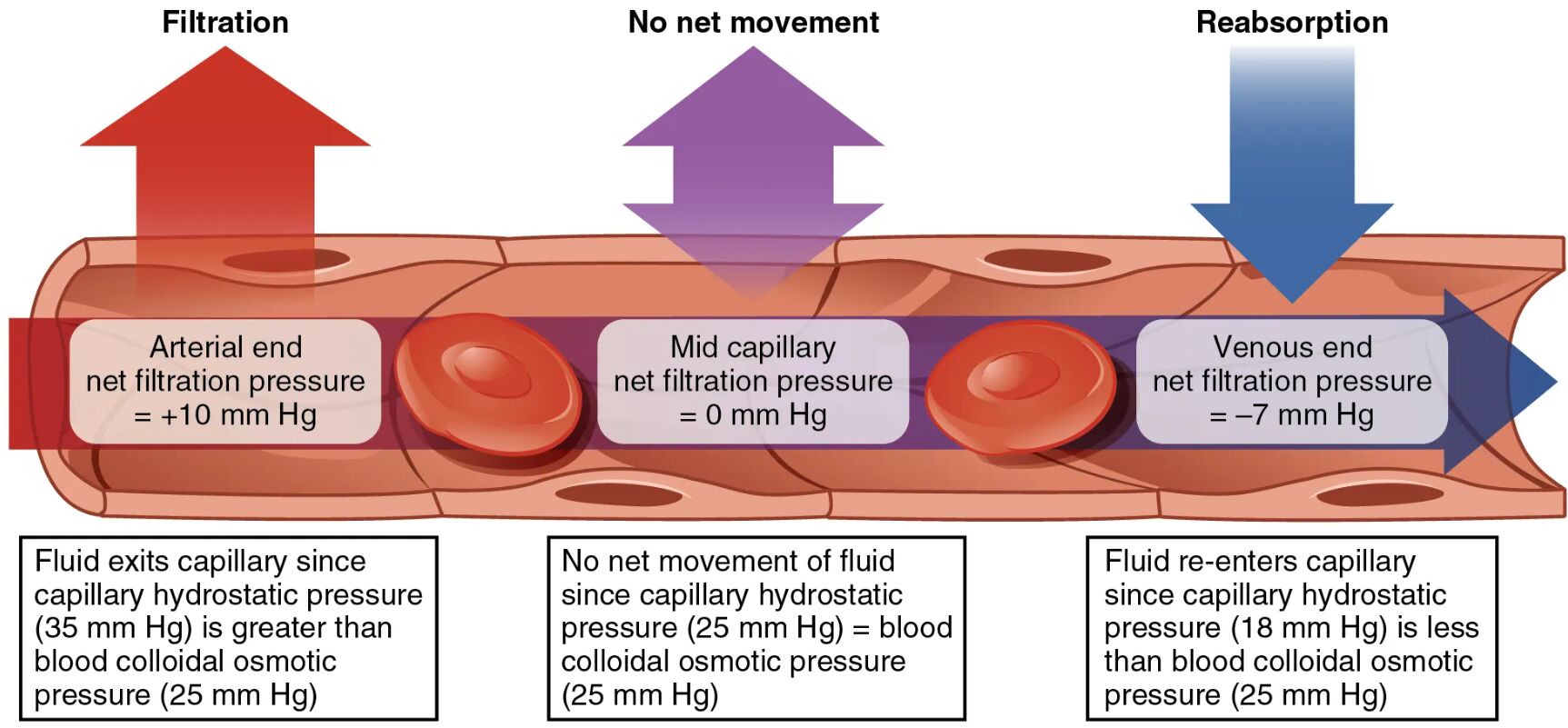
Filtration Filtration occurs at the arterial end of the capillary, where fluid exits due to a positive net filtration pressure of +10 mmHg. This process is driven by the higher capillary hydrostatic pressure, allowing plasma and small solutes to move into the interstitial space.
No net movement No net movement is observed at the mid-capillary region, where the net filtration pressure is 0 mmHg due to equal capillary hydrostatic pressure (25 mmHg) and blood colloidal osmotic pressure (25 mmHg). This equilibrium prevents significant fluid shift in either direction at this point.
Reabsorption Reabsorption takes place at the venous end, where fluid re-enters the capillary due to a negative net filtration pressure of -7 mmHg. This occurs because the blood colloidal osmotic pressure exceeds the reduced capillary hydrostatic pressure, pulling fluid back into the vessel.
Arterial end net filtration pressure Arterial end net filtration pressure is +10 mmHg, reflecting the dominance of capillary hydrostatic pressure (35 mmHg) over blood colloidal osmotic pressure (25 mmHg). This positive pressure gradient facilitates the outward movement of fluid at the capillary’s beginning.
Mid capillary net filtration pressure Mid capillary net filtration pressure is 0 mmHg, indicating a balance between capillary hydrostatic pressure (25 mmHg) and blood colloidal osmotic pressure (25 mmHg). This balance halts net fluid movement, marking a transitional zone in the capillary.
Venous end net filtration pressure Venous end net filtration pressure is -7 mmHg, resulting from a capillary hydrostatic pressure (18 mmHg) lower than blood colloidal osmotic pressure (25 mmHg). This negative pressure drives fluid reabsorption back into the capillary toward the venous end.
Overview of Capillary Exchange
The diagram provides a clear depiction of how fluid moves across capillary walls based on pressure gradients. This process is essential for maintaining tissue homeostasis and supporting metabolic functions.
- Filtration at the arterial end supports nutrient delivery and waste removal from tissues.
- No net movement at the midpoint reflects a critical balance point in pressure dynamics.
- Reabsorption at the venous end ensures fluid return to the bloodstream, preventing edema.
- Arterial end net filtration pressure, mid capillary net filtration pressure, and venous end net filtration pressure guide the directionality of fluid shift.
- The interplay of hydrostatic and osmotic pressures governs this exchange process.
The Role of Pressure in Fluid Movement
Pressure differences across the capillary wall determine the direction of fluid flow. Understanding these forces enhances comprehension of capillary function.
- Filtration occurs when capillary hydrostatic pressure (35 mmHg) exceeds blood colloidal osmotic pressure (25 mmHg) at the arterial end.
- No net movement happens as capillary hydrostatic pressure drops to 25 mmHg, equaling osmotic pressure.
- Reabsorption begins when capillary hydrostatic pressure falls to 18 mmHg, allowing osmotic pressure to dominate.
- Arterial end net filtration pressure of +10 mmHg reflects the initial high driving force.
- Venous end net filtration pressure of -7 mmHg indicates the reabsorption phase’s strength.
Hydrostatic and Osmotic Pressure Dynamics
Hydrostatic and osmotic pressures work in opposition to regulate fluid exchange. Their balance is key to maintaining capillary integrity.
- Filtration is driven by capillary hydrostatic pressure, generated by arterial blood flow.
- No net movement occurs when these pressures neutralize, typically mid-capillary.
- Reabsorption relies on blood colloidal osmotic pressure, created by plasma proteins like albumin.
- Arterial end net filtration pressure decreases as blood flows, reducing hydrostatic pressure.
- Venous end net filtration pressure shifts due to lower hydrostatic pressure and constant osmotic pull.
Clinical Implications of Capillary Exchange
Variations in capillary exchange can signal health issues or guide treatment strategies. Monitoring these pressures aids in managing fluid balance.
- Excessive filtration may lead to edema if hydrostatic pressure rises, as in heart failure.
- Impaired reabsorption due to low osmotic pressure can occur in malnutrition or liver disease.
- No net movement disruption might indicate capillary damage, affecting exchange efficiency.
- Arterial end net filtration pressure changes can reflect arterial hypertension or stenosis.
- Venous end net filtration pressure alterations may suggest venous insufficiency or thrombosis.
In conclusion, the capillary exchange diagram offers a window into the delicate balance of filtration, no net movement, and reabsorption, driven by arterial end net filtration pressure, mid capillary net filtration pressure, and venous end net filtration pressure. This process underscores the body’s ability to regulate fluid and nutrient exchange, supporting tissue health and overall circulatory function. Understanding these dynamics provides a solid foundation for addressing fluid-related conditions and optimizing patient care.

