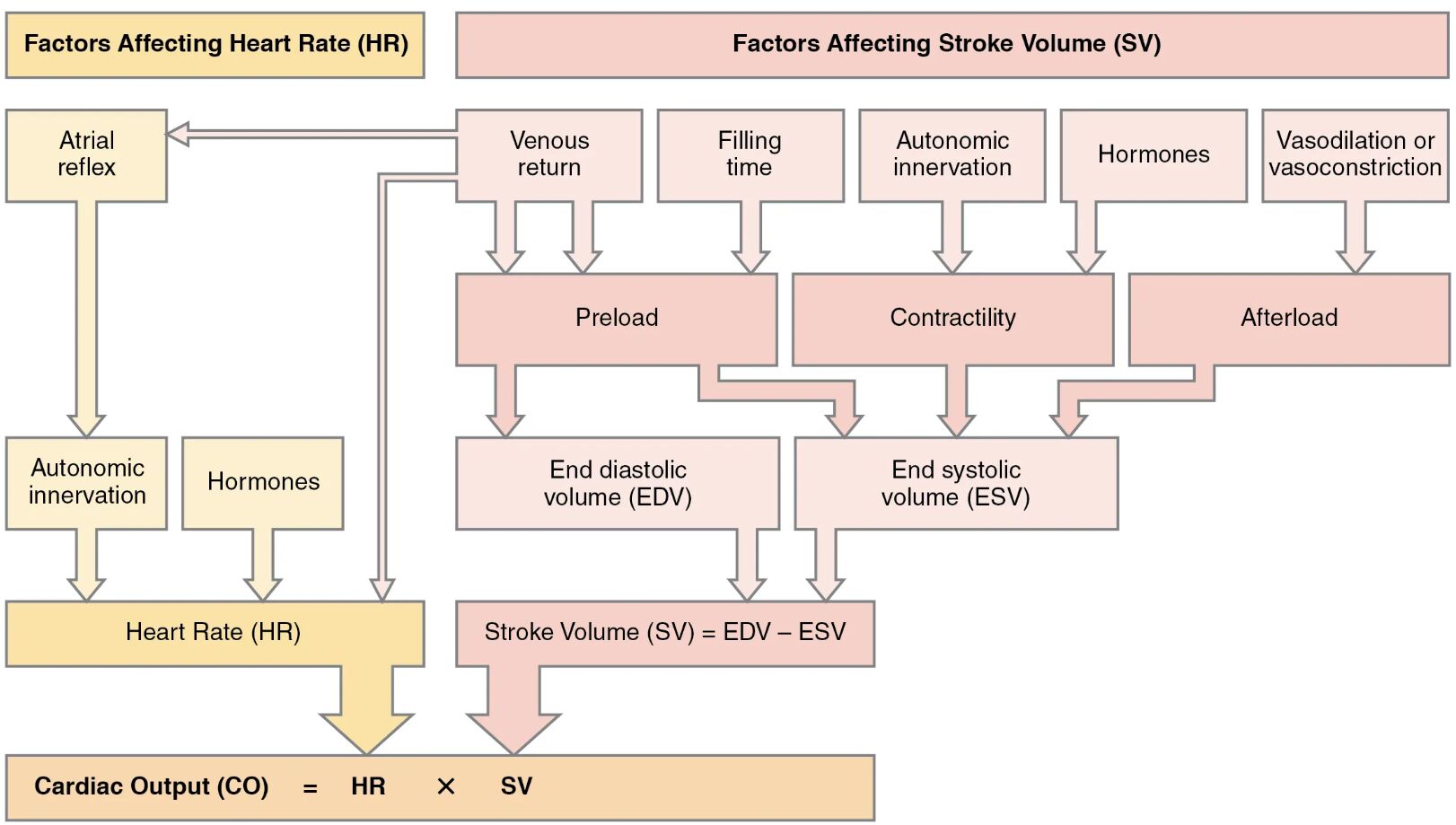
Delve into the intricate mechanisms that regulate cardiac output, a critical measure of heart performance that reflects the amount of blood the heart pumps per minute. This comprehensive guide explores the primary factors affecting heart rate and stroke volume, illustrated through a detailed diagram, to provide a clear understanding of cardiovascular physiology. Whether you’re exploring the autonomic nervous system’s role or the impact of hormonal influences, this article breaks down the essentials for a thorough grasp of how the heart maintains efficient circulation.
Label Introduction
- Atrial reflex The atrial reflex is a key mechanism that helps regulate heart rate by responding to changes in blood pressure within the atria. It triggers an increase in heart rate when venous return increases, ensuring the heart adapts to the body’s demands.
- Venous return Venous return refers to the volume of blood flowing back to the heart, which directly influences the preload and subsequently the heart’s filling. Adequate venous return is essential for maintaining optimal cardiac output during various physiological states.
- Filling time Filling time is the duration available for the ventricles to fill with blood during diastole, impacting the end-diastolic volume. Insufficient filling time can reduce stroke volume, especially during rapid heart rates.
- Autonomic innervation Autonomic innervation involves the sympathetic and parasympathetic nervous systems that modulate heart rate and contractility. The balance between these systems fine-tunes the heart’s response to stress or rest.
- Hormones Hormones, such as epinephrine and norepinephrine, are released by the adrenal glands to increase heart rate and contractility during the “fight or flight” response. Thyroid hormones like T3 and T4 also play a longer-term role in regulating metabolic demand and cardiac function.
- Vasodilation or vasoconstriction Vasodilation or vasoconstriction refers to the widening or narrowing of blood vessels, respectively, which affects afterload by altering peripheral resistance. This process influences the workload on the heart and the ease of blood ejection.
- Preload Preload is the initial stretching of the cardiac myocytes prior to contraction, determined by the end-diastolic volume. An increase in preload, often due to greater venous return, enhances the force of contraction via the Frank-Starling mechanism.
- Contractility Contractility is the intrinsic ability of the heart muscle to contract, influenced by factors like calcium availability and sympathetic stimulation. Enhanced contractility increases the stroke volume by improving the heart’s pumping efficiency.
- Afterload Afterload is the resistance the heart must overcome to eject blood into the aorta and pulmonary arteries, primarily affected by arterial pressure. High afterload can reduce stroke volume if it exceeds the heart’s contractile strength.
- End diastolic volume (EDV) End diastolic volume is the volume of blood in the ventricles at the end of diastole, serving as a measure of preload. It sets the stage for the subsequent contraction and is a critical determinant of stroke volume.
- End systolic volume (ESV) End systolic volume is the volume of blood remaining in the ventricles after systole, reflecting the efficiency of contraction. A lower ESV indicates a higher stroke volume, contributing to effective cardiac output.
- Heart Rate (HR) Heart rate is the number of beats per minute, regulated by autonomic innervation and hormonal influences. It directly determines the frequency of cardiac cycles and is a key component of cardiac output.
- Stroke Volume (SV) Stroke volume is the amount of blood pumped out of the left ventricle per beat, calculated as the difference between EDV and ESV. It is influenced by preload, contractility, and afterload, playing a pivotal role in cardiac performance.
- Cardiac Output (CO) Cardiac output is the total volume of blood the heart pumps per minute, expressed as the product of heart rate and stroke volume. It is a vital indicator of cardiovascular health and adjusts to meet the body’s metabolic needs.
Overview of Cardiac Output and Its Importance
Understanding cardiac output is fundamental to grasping how the heart sustains life by delivering oxygen and nutrients. The heart’s ability to adapt to varying physiological demands relies on the interplay of heart rate and stroke volume. This diagram provides a visual roadmap to the factors at play, making it an invaluable tool for learning cardiovascular dynamics.
- Explains the basic formula: CO = HR × SV, highlighting its reliance on two primary components.
- Details how changes in either heart rate or stroke volume can significantly impact overall cardiac output.
- Discusses the role of the cardiovascular system in maintaining homeostasis under different conditions.
Factors Influencing Heart Rate
Heart rate regulation is a complex process involving multiple physiological controls. The autonomic nervous system and endocrine system work in tandem to adjust heart rate based on the body’s needs.
- Describes how the atrial reflex responds to atrial stretch, increasing heart rate during heightened venous return.
- Outlines the role of autonomic innervation, with the sympathetic system accelerating and the parasympathetic slowing heart rate.
- Highlights how hormones like epinephrine provide rapid adjustments during stress, while thyroid hormones influence baseline rates.
Factors Influencing Stroke Volume
Stroke volume is determined by the heart’s filling and pumping efficiency, influenced by several key factors. These elements ensure the heart can adapt to varying workloads and maintain adequate blood flow.
- Explores preload as a determinant of how much the heart stretches before contraction, governed by venous return and filling time.
- Examines contractility, where increased calcium and sympathetic input enhance the heart’s pumping strength.
- Analyzes afterload, where vascular resistance affects the ease of blood ejection, impacting stroke volume.
The Role of Preload, Contractility, and Afterload
These three factors are the cornerstone of stroke volume regulation, each contributing uniquely to cardiac performance. Their balance ensures the heart can respond effectively to physiological demands.
- Details how preload increases with greater end-diastolic volume, enhancing contraction via the Frank-Starling law.
- Discusses contractility improvements with positive inotropic agents like digoxin, boosting stroke volume.
- Explains how afterload rises with hypertension, potentially reducing stroke volume if not counterbalanced.
Clinical Implications and Physiological Adaptations
The factors affecting cardiac output have significant clinical relevance, especially in conditions like heart failure. Understanding these dynamics aids in diagnosing and managing cardiovascular health.
- Notes how altered venous return due to dehydration can decrease preload and cardiac output.
- Addresses how enhanced contractility with inotropic support can aid failing hearts.
- Considers how vasodilation or vasoconstriction therapies adjust afterload to optimize cardiac function.
Integrating Heart Rate and Stroke Volume
The synergy between heart rate and stroke volume defines cardiac output, adapting to exercise, rest, and stress. This integration ensures the heart meets the body’s oxygen demands efficiently.
- Illustrates how increased heart rate (HR) during exercise boosts cardiac output alongside stroke volume.
- Shows how stroke volume (SV) adjustments compensate for changes in heart rate to maintain output.
- Emphasizes the role of cardiac output (CO) as a dynamic measure reflecting overall cardiovascular status.
Practical Applications in Cardiovascular Health
Knowledge of these factors aids in monitoring and enhancing heart function in various settings. From athletic training to medical interventions, this understanding is crucial.
- Suggests monitoring heart rate (HR) and stroke volume (SV) during exercise to optimize performance.
- Recommends assessing preload and afterload in patients with circulatory issues.
- Highlights the importance of cardiac output (CO) measurements in critical care scenarios.
In conclusion, mastering the factors influencing cardiac output provides a solid foundation for understanding cardiovascular physiology. The interplay of heart rate and stroke volume, driven by autonomic, hormonal, and mechanical factors, ensures the heart adapts to the body’s ever-changing needs. This diagram serves as a valuable reference, offering insights into the heart’s remarkable ability to maintain circulation under diverse conditions.

