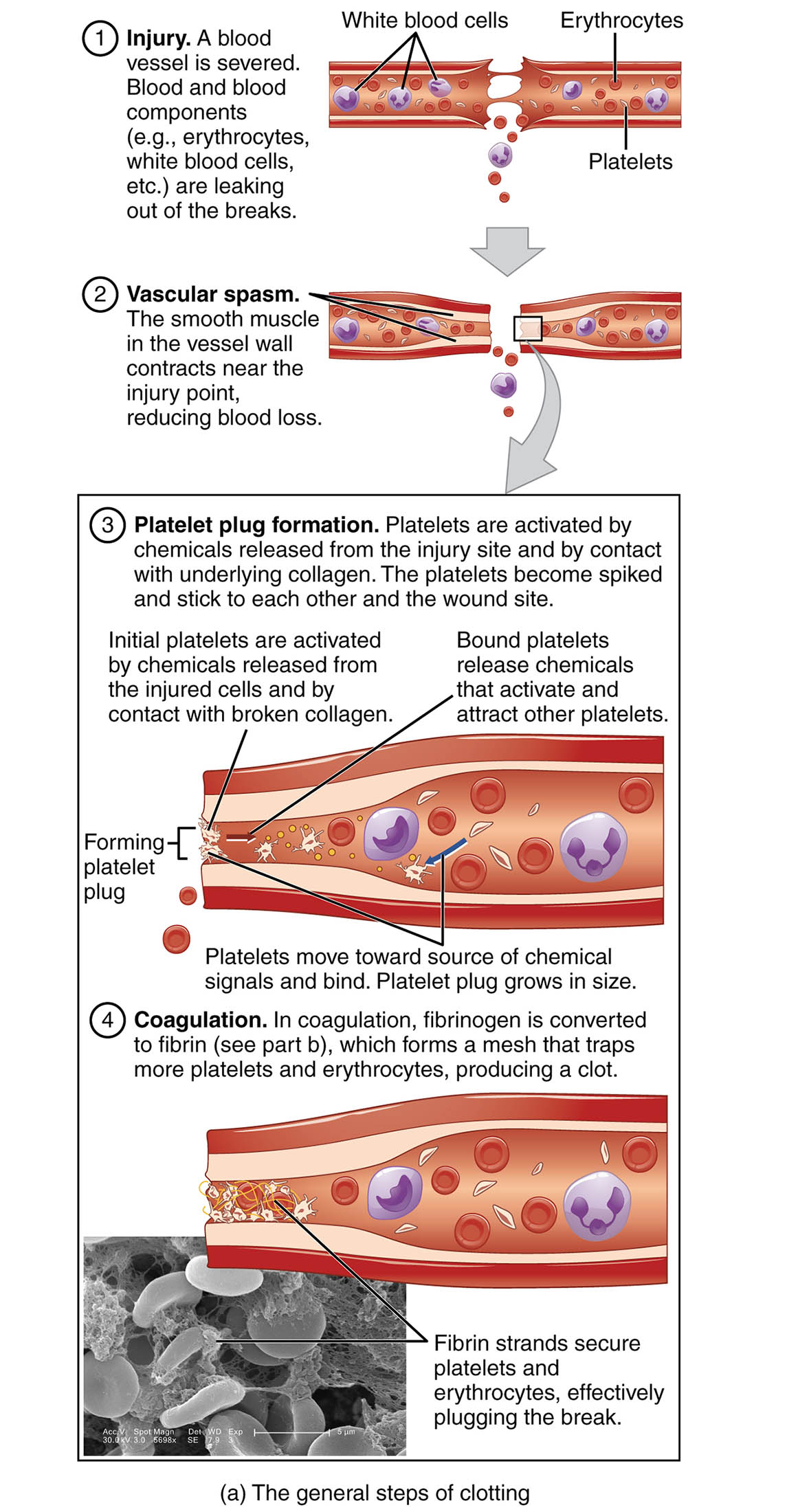
The process of hemostasis is a critical mechanism in the human body that prevents excessive bleeding when a blood vessel is injured. This intricate process involves a series of coordinated steps, including vascular spasm, platelet plug formation, and coagulation, each playing a vital role in sealing the wound and repairing the vessel. The accompanying diagram illustrates these stages clearly, offering a visual guide to how the body naturally manages blood loss and maintains circulatory integrity.
Injury
- This initial stage occurs when a blood vessel is severed, leading to the immediate leakage of blood components such as erythrocytes, white blood cells, and platelets.
- The disruption triggers the body’s rapid response to minimize blood loss and initiate the healing process.
Vascular spasm
- The smooth muscle in the vessel wall contracts near the injury point, reducing blood flow and helping to limit the extent of bleeding.
- This temporary constriction is a crucial first defense mechanism to stabilize the injury site.
Platelet plug formation
- Platelets are activated by chemicals released from the injury site and by contact with underlying collagen, causing them to become spiked and adhere to each other and the wound site.
- Initial platelets are activated by chemicals from injured cells and collagen contact, while bound platelets release chemicals that attract and activate additional platelets, forming a growing plug.
Coagulation
- In this phase, fibrinogen is converted to fibrin, which forms a mesh that traps more platelets and erythrocytes, producing a stable clot.
- Fibrin strands secure platelets and erythrocytes effectively, plugging the leak and facilitating vessel wall repair once bleeding has stopped.
Blood clotting, or hemostasis, is a fascinating and essential process that ensures the body can respond effectively to vascular injuries. The diagram above provides a detailed visual representation of the three primary stages involved: vascular spasm, platelet plug formation, and coagulation. Understanding these steps is key to appreciating how the body maintains its circulatory balance and prevents life-threatening blood loss.
Vascular Spasm: The First Line of Defense
The vascular spasm stage begins the moment a blood vessel is injured, setting the stage for subsequent clotting mechanisms. This process involves the smooth muscle within the vessel walls contracting to reduce blood flow, effectively minimizing the initial loss.
- The contraction is triggered by local nerve reflexes and chemical signals released at the injury site.
- This rapid response helps to stabilize the area, preparing it for the formation of a platelet plug.
Platelet Plug Formation: Building the Temporary Seal
Following the vascular spasm, platelet plug formation takes over as the next critical step in hemostasis. Platelets, small cell fragments in the blood, become activated and aggregate to form a temporary barrier at the injury site.
- Activation occurs when platelets encounter exposed collagen and chemicals from damaged tissues, causing them to change shape and stick together.
- The growing platelet plug is reinforced as additional platelets are recruited, creating a foundation for the coagulation phase.
Coagulation: Solidifying the Clot
The final stage, coagulation, transforms the temporary platelet plug into a stable, long-lasting clot. This process involves a complex cascade of reactions that ultimately produce fibrin, a strong protein mesh.
- Fibrinogen, a soluble plasma protein, is converted into insoluble fibrin strands by the enzyme thrombin, which is generated during the clotting cascade.
- These fibrin strands entangle platelets, erythrocytes, and other blood components, forming a robust clot that seals the vessel and supports healing.
Hemostasis is a remarkable example of the body’s ability to protect itself from excessive bleeding. The process begins with an injury to a blood vessel, which disrupts the normal flow of blood and exposes underlying tissues. Vascular spasm immediately reduces blood loss by constricting the vessel, a response mediated by smooth muscle contraction and neurochemical signals. This initial step is crucial, as it buys time for the more complex processes of platelet plug formation and coagulation to take effect.
Platelet plug formation involves the activation of platelets, which are essential for initiating clot formation. When a vessel is damaged, the exposed collagen and released chemicals signal platelets to adhere to the site and to each other, forming a temporary seal. This plug grows as more platelets are attracted and activated, creating a barrier that prevents further blood loss. The efficiency of this step depends on the rapid response of platelets and their ability to interact with the vessel wall.
Coagulation completes the hemostasis process by stabilizing the platelet plug through the formation of a fibrin network. This stage involves a series of enzymatic reactions, known as the coagulation cascade, which culminate in the conversion of fibrinogen to fibrin. The resulting mesh traps additional blood cells and platelets, forming a solid clot that not only seals the injury but also provides a scaffold for tissue repair. Once the vessel wall is repaired and the leakage stops, the clot is gradually broken down by the body’s fibrinolytic system.
The process of hemostasis is tightly regulated to ensure it occurs only where needed and does not lead to unwanted clot formation, such as in deep vein thrombosis or pulmonary embolism. Key players like thrombin and fibrin work in harmony with platelets and vascular components to maintain this balance. For those studying the circulatory system, understanding these mechanisms provides insight into both normal physiology and potential pathological conditions.

