Explore the characteristics of sinus bradycardia on an electrocardiogram (ECG), focusing on its presentation in Lead II and typical heart rate. This article provides detailed insights into this common cardiac rhythm, its physiological causes, and when it may signify a clinical concern.
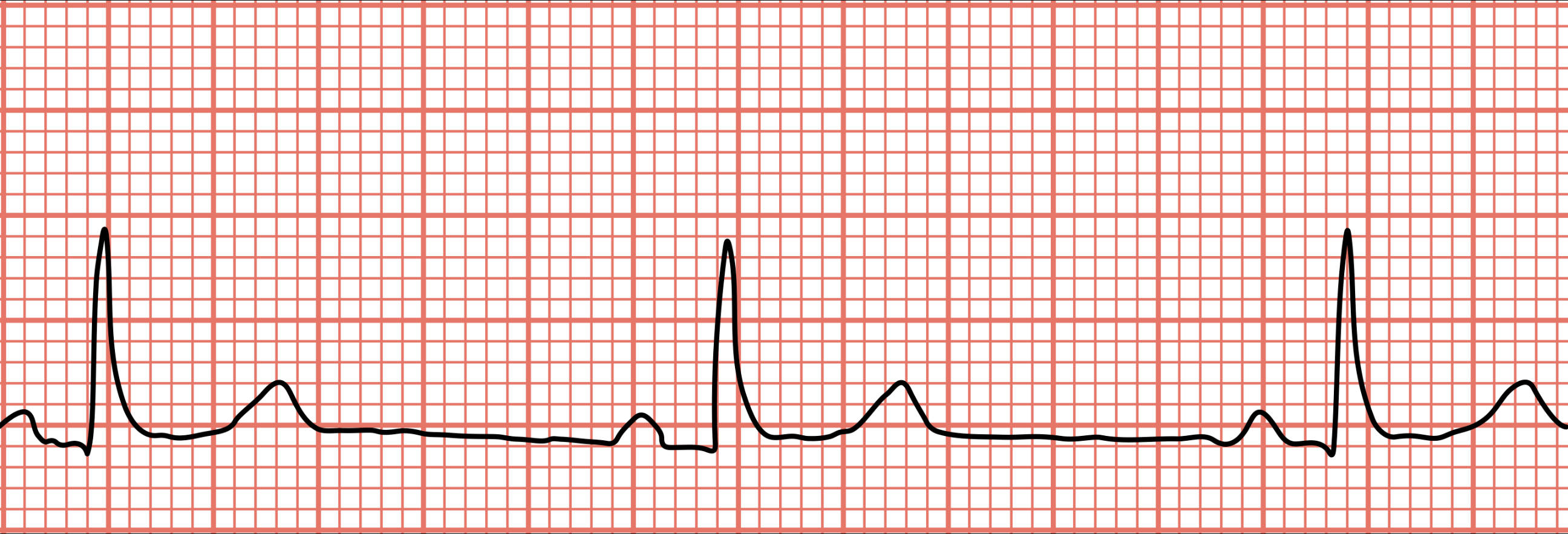
Sinus bradycardia as seen in lead 2. HR about 50: This describes the specific cardiac rhythm displayed in the electrocardiogram (ECG) tracing, indicating a heart rate of approximately 50 beats per minute. Observing this pattern in Lead II is a standard method for assessing cardiac rhythm.
Sinus bradycardia seen in lead II with a heart rate of about 50 BPM: This reiterates the presence of sinus bradycardia, with the heart rate explicitly stated as 50 beats per minute. This information is crucial for accurately diagnosing the rhythm and assessing its clinical significance.
An electrocardiogram (ECG or EKG) is a fundamental diagnostic tool in cardiology, offering a non-invasive window into the heart’s electrical activity. By recording the tiny electrical impulses that govern each heartbeat, an ECG provides crucial information about the heart’s rhythm, rate, and conduction system. Among the many cardiac rhythms, sinus bradycardia is a common finding, characterized by a slow heart rate originating from the sinoatrial (SA) node, the natural pacemaker of the heart. While often benign, understanding its presentation and potential implications is vital for medical professionals.
The ECG tracing provided clearly illustrates a classic example of sinus bradycardia, specifically as seen in Lead II, with a heart rate of approximately 50 beats per minute (BPM). This rhythm is defined by a heart rate below 60 BPM, originating from the SA node, and is characterized by normal P waves preceding every QRS complex, with a consistent PR interval. Recognizing this pattern is the first step in determining its clinical significance and deciding on appropriate management, if any.
While sinus bradycardia can sometimes signal an underlying health issue, it is also a common and often normal physiological finding. For instance, well-trained athletes frequently exhibit resting heart rates in the 40s or 50s due to enhanced vagal tone, a sign of excellent cardiovascular fitness. Understanding the context in which sinus bradycardia is observed is therefore crucial for accurate interpretation.
- Sinus bradycardia is a heart rate below 60 BPM, originating from the SA node.
- It is characterized by normal P waves before each QRS complex.
- Often a normal finding in athletes or during sleep.
- Can be caused by medications, certain medical conditions, or vagal stimulation.
The hallmark of sinus bradycardia on an ECG is a slow, regular rhythm, where each QRS complex is preceded by a P wave that originates from the sinoatrial node. This means the P wave will be upright in Lead II, indicating normal atrial depolarization. The PR interval, representing the time it takes for the electrical impulse to travel from the atria to the ventricles, should be within the normal range (0.12-0.20 seconds). The QRS complex, which depicts ventricular depolarization, should also appear normal in duration and morphology unless there is an underlying conduction defect. In the provided image, the regular spacing between the QRS complexes and the clear P waves preceding each one, along with a rate of 50 BPM, confirm the diagnosis.
The causes of sinus bradycardia are diverse. Physiologically, it can be a normal variant in highly conditioned athletes due to increased vagal tone, which slows the SA node firing rate. It also commonly occurs during sleep. Pathological causes include medications such as beta-blockers, calcium channel blockers, and certain antiarrhythmic drugs. Hypothyroidism, sick sinus syndrome (a dysfunction of the SA node itself), increased intracranial pressure, and electrolyte imbalances can also lead to sinus bradycardia. Additionally, conditions that increase vagal stimulation, such as severe pain, straining, or carotid sinus massage, can temporarily slow the heart rate.
Clinically, the significance of sinus bradycardia depends on whether it is symptomatic. Many individuals with a heart rate of 50 BPM, especially if physically active, may be entirely asymptomatic. However, if the bradycardia is severe enough to reduce cardiac output, patients may experience symptoms such as dizziness, fatigue, syncope (fainting), shortness of breath, or chest pain. In such symptomatic cases, further investigation is warranted to identify the underlying cause and determine appropriate treatment. Treatment options can range from discontinuing offending medications to implanting a permanent pacemaker for severe, persistent symptomatic bradycardia due to intrinsic SA node dysfunction.
In conclusion, sinus bradycardia is a common ECG finding characterized by a heart rate below 60 BPM with normal P waves and consistent PR intervals. While frequently a benign physiological variation, particularly in athletes, it can also be indicative of underlying medical conditions or medication side effects. Accurate interpretation of the ECG, coupled with a thorough clinical evaluation for symptoms, is paramount for distinguishing between a normal variant and a clinically significant bradycardia requiring intervention. Understanding this fundamental cardiac rhythm is essential for all healthcare professionals involved in patient care.

