Explore the critical connection between bradycardia, a slower-than-normal heart rate, and episodes of fainting, medically known as syncope. This article delves into the physiological mechanisms behind these events, highlighting how a compromised heart rhythm can lead to insufficient blood flow to the brain. Gain insights into the causes, symptoms, and potential implications of bradycardia-induced fainting for overall cardiovascular health.
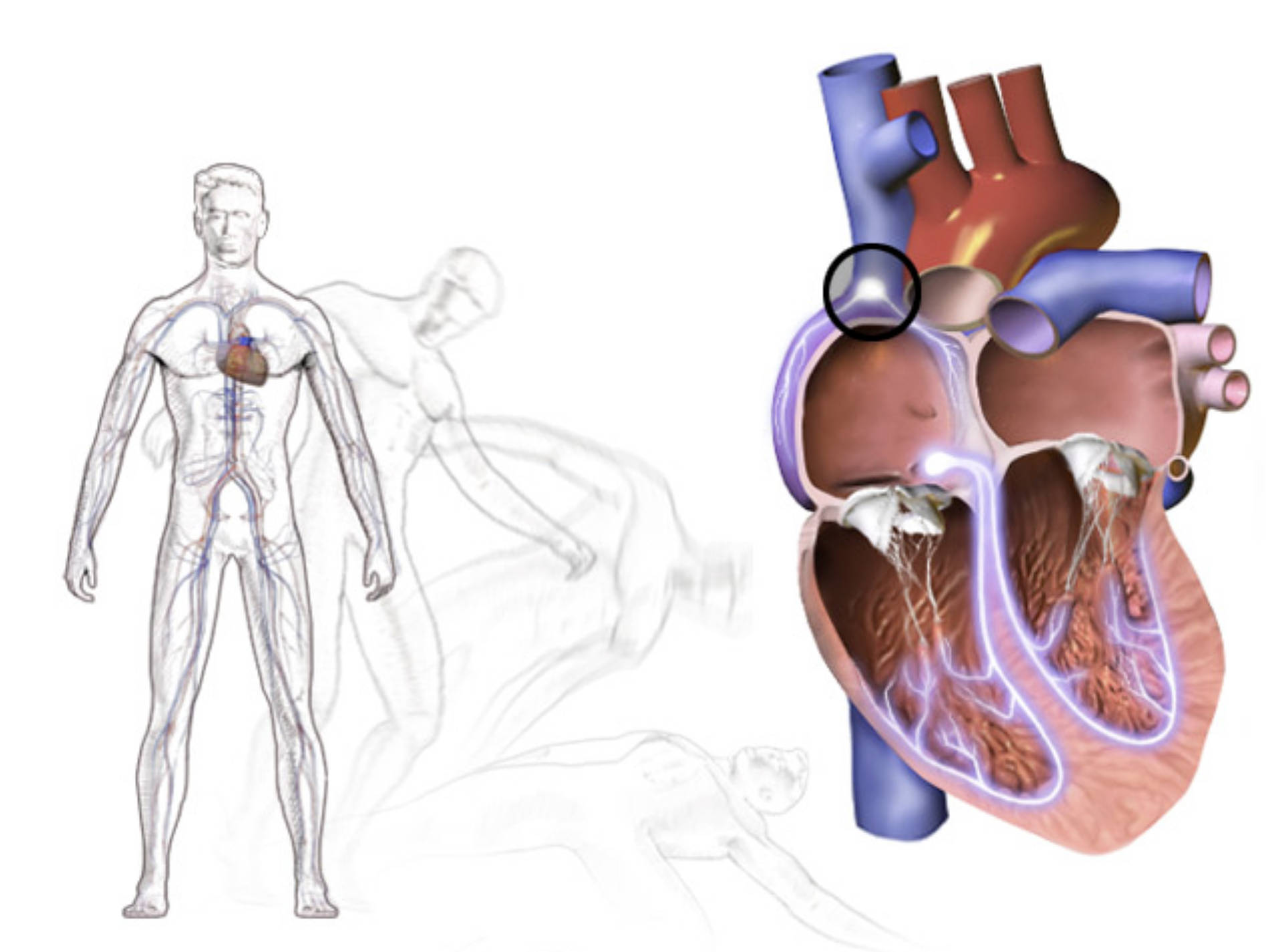
Fainting, or syncope, is a temporary loss of consciousness caused by a sudden, transient decrease in blood flow to the brain. While various factors can trigger syncope, one significant underlying cause is bradycardia, a condition characterized by a heart rate that is abnormally slow. A healthy adult’s resting heart rate typically ranges from 60 to 100 beats per minute (bpm). When the heart beats significantly slower than this, it may not be able to pump enough oxygen-rich blood to meet the body’s demands, particularly those of the brain. The image illustrates the systemic circulatory system and a cross-section of the heart, where a circled area might indicate a point of origin for an electrical issue leading to bradycardia.
What is Bradycardia?
Bradycardia is defined as a resting heart rate of less than 60 bpm, although what constitutes “too slow” can vary among individuals and depend on fitness levels (e.g., highly trained athletes often have lower resting heart rates). The heart’s electrical system, which dictates its rhythm, originates with the sinoatrial (SA) node, the natural pacemaker. If the SA node malfunctions, or if electrical signals are blocked or delayed as they travel through the heart, bradycardia can occur. This can lead to symptoms like dizziness, fatigue, shortness of breath, and importantly, syncope.
Causes of Bradycardia
Bradycardia can stem from a variety of causes, ranging from benign to potentially life-threatening. Common causes include:
- Age-related degeneration: As people age, the SA node or other parts of the heart’s electrical system can wear down.
- Heart conditions: Damage to heart tissue from a heart attack, heart disease, or congenital heart defects can impair electrical pathways.
- Medications: Certain drugs, such as beta-blockers, calcium channel blockers, and antiarrhythmics, can slow the heart rate.
- Hypothyroidism: An underactive thyroid gland can reduce metabolic rate, including heart rate.
- Electrolyte imbalances: Disturbances in potassium, calcium, or other electrolytes can affect heart rhythm.
- Infections: Myocarditis, an inflammation of the heart muscle, can disrupt electrical signals.
- Obstructive sleep apnea: This condition can lead to drops in heart rate during sleep.
- Vasovagal syncope: A common type of fainting triggered by a sudden drop in heart rate and blood pressure, often due to emotional stress or prolonged standing.
The Mechanism of Fainting in Bradycardia
When the heart rate slows significantly due to bradycardia, the cardiac output—the amount of blood pumped by the heart per minute—decreases. This reduction in cardiac output directly leads to a decrease in systemic blood pressure. If the blood pressure falls below a critical threshold, insufficient blood reaches the brain. Brain cells are highly sensitive to oxygen deprivation; even a few seconds of inadequate blood supply can cause a temporary loss of brain function, resulting in fainting. The body’s natural response to fainting is to fall to a horizontal position, which helps to restore blood flow to the brain by eliminating the need to pump against gravity.
Understanding the link between bradycardia and fainting is crucial for proper diagnosis and management. While an occasional fainting episode might be benign, recurrent syncope, especially when associated with a slow heart rate, warrants immediate medical evaluation. Diagnostic tools like electrocardiograms (ECGs), Holter monitors, or event recorders can help identify the underlying cause of bradycardia. Treatment strategies vary depending on the cause and severity, ranging from medication adjustments to the implantation of a pacemaker to regulate the heart’s rhythm. Early detection and intervention are key to preventing complications and improving patient outcomes.

