The human body maintains a delicate balance through autoregulation and homeostasis, processes that ensure tissues receive adequate blood flow under varying conditions. This diagram illustrates how local receptors detect changes and trigger responses involving vasodilators and vasoconstrictors, ultimately stabilizing circulation to support overall health.
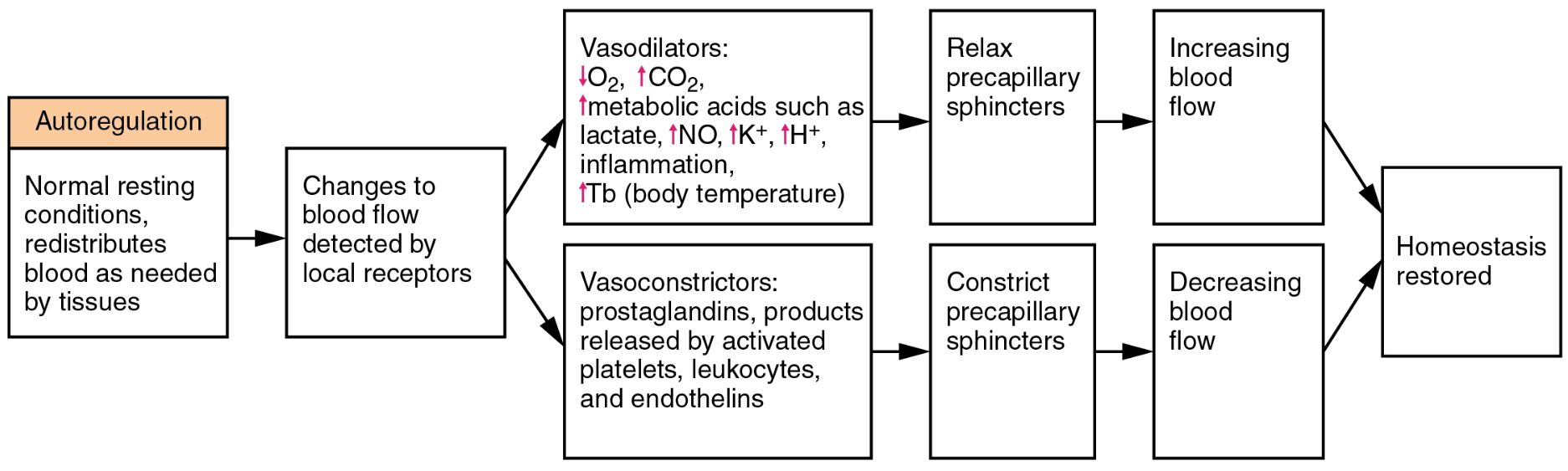
Autoregulation This intrinsic mechanism allows tissues to control their own blood supply based on metabolic needs. It adjusts vascular tone to redistribute blood flow, ensuring optimal oxygen and nutrient delivery even during rest or activity.
Normal resting conditions, redistributes blood as needed by tissues Under typical physiological states, the body fine-tunes blood distribution to match tissue demands. This process involves sensing local conditions and responding dynamically to maintain equilibrium.
Changes to blood flow detected by local receptors Local sensors monitor shifts in blood flow caused by metabolic or environmental factors. These receptors then signal the vascular system to initiate corrective actions to preserve tissue function.
Vasodilators: ↓O₂, ↑CO₂, ↑metabolic acids such as lactate, ↑NO, ↑K⁺, ↑H⁺, inflammation, ↑Tb (body temperature) These substances and conditions signal the need for increased blood flow by relaxing vessels. For instance, reduced oxygen levels or elevated carbon dioxide prompt vasodilation to enhance perfusion.
Relax precapillary sphincters Relaxation of these muscular gates increases blood flow into capillary beds. This adjustment ensures that tissues with higher metabolic demands receive adequate supply.
Increasing blood flow Enhanced flow delivers oxygen and nutrients where needed most. This response supports cellular activity and prevents hypoxia during periods of increased demand.
Vasoconstrictors: prostaglandins, products released by activated platelets, leukocytes, and endothelins These agents reduce blood flow by narrowing vessels in response to certain signals. They help redirect blood to more critical areas when local needs decrease.
Constrict precapillary sphincters Tightening these sphincters limits blood entry into specific capillary beds. This mechanism conserves blood volume for other regions requiring support.
Decreasing blood flow Reduced flow conserves resources and prevents over-perfusion in areas with lower metabolic activity. It plays a key role in maintaining systemic balance.
Homeostasis restored Through these adjustments, the body returns to a stable state, ensuring consistent internal conditions. This restoration supports long-term health and resilience.
The Role of Autoregulation in Circulation
Autoregulation is a vital process that maintains blood flow despite changes in systemic pressure. It ensures that organs like the brain and kidneys receive steady perfusion through localized control.
- The mechanism operates independently of central nervous system input, relying on myogenic and metabolic responses.
- Myogenic response involves smooth muscle contraction in response to stretch, stabilizing flow in arteries.
- Metabolic factors, such as lactic acid buildup, trigger vasodilation to meet tissue oxygen needs.
- This process is crucial during exercise when muscle blood flow must increase rapidly.
- Hormonal influences, like nitric oxide, enhance vasodilation to support metabolic demand.
How Local Receptors Detect Changes
Changes to blood flow detected by local receptors serve as the body’s early warning system. These sensors respond to chemical and physical cues to initiate autoregulatory responses.
- Decreased oxygen levels signal hypoxia, prompting immediate vasodilation.
- Elevated carbon dioxide or hydrogen ions indicate metabolic stress, triggering flow adjustments.
- Temperature changes, such as fever, influence vascular tone to redistribute heat.
- Inflammatory mediators like prostaglandins activate receptors during injury or infection.
- This sensitivity ensures rapid adaptation to maintain tissue viability.
Vasodilators and Their Impact
Vasodilators play a key role in relaxing precapillary sphincters to boost blood flow. They respond to specific metabolic signals to optimize circulation.
- Nitric oxide, released by endothelial cells, promotes smooth muscle relaxation.
- Increased potassium and hydrogen ions reflect cellular activity, necessitating more flow.
- Lactate accumulation during anaerobic metabolism signals the need for oxygen delivery.
- Carbon dioxide buildup, a byproduct of respiration, drives vasodilation in active tissues.
- These actions collectively enhance nutrient supply and waste removal.
Vasoconstrictors and Flow Reduction
Vasoconstrictors, including endothelins, help constrict precapillary sphincters to decrease blood flow. This response redirects circulation to prioritize vital organs.
- Prostaglandins from activated platelets initiate vasoconstriction during clotting.
- Leukocyte-derived products contribute to vascular narrowing in inflammation.
- Endothelins, potent peptides, regulate flow in response to stress or injury.
- This mechanism prevents excessive bleeding and maintains pressure in other areas.
- Balanced action ensures efficient resource allocation across the body.
Achieving Homeostasis Through Feedback
The interplay of increasing and decreasing blood flow ultimately restores homeostasis. This feedback loop maintains optimal internal conditions for all tissues.
- Enhanced flow during exercise supports muscle oxygen demand, then subsides at rest.
- Reduced flow in inactive regions conserves energy and prevents edema.
- The system adjusts dynamically to hormonal signals like adrenaline surges.
- Long-term stability prevents conditions like ischemia or hyperemia.
- Understanding this balance aids in managing circulatory health effectively.
The intricate dance of autoregulation and homeostasis underscores the body’s ability to adapt to changing needs. By fine-tuning blood flow through local and systemic mechanisms, the circulatory system ensures every tissue thrives, offering a foundation for further exploration into physiological resilience.

