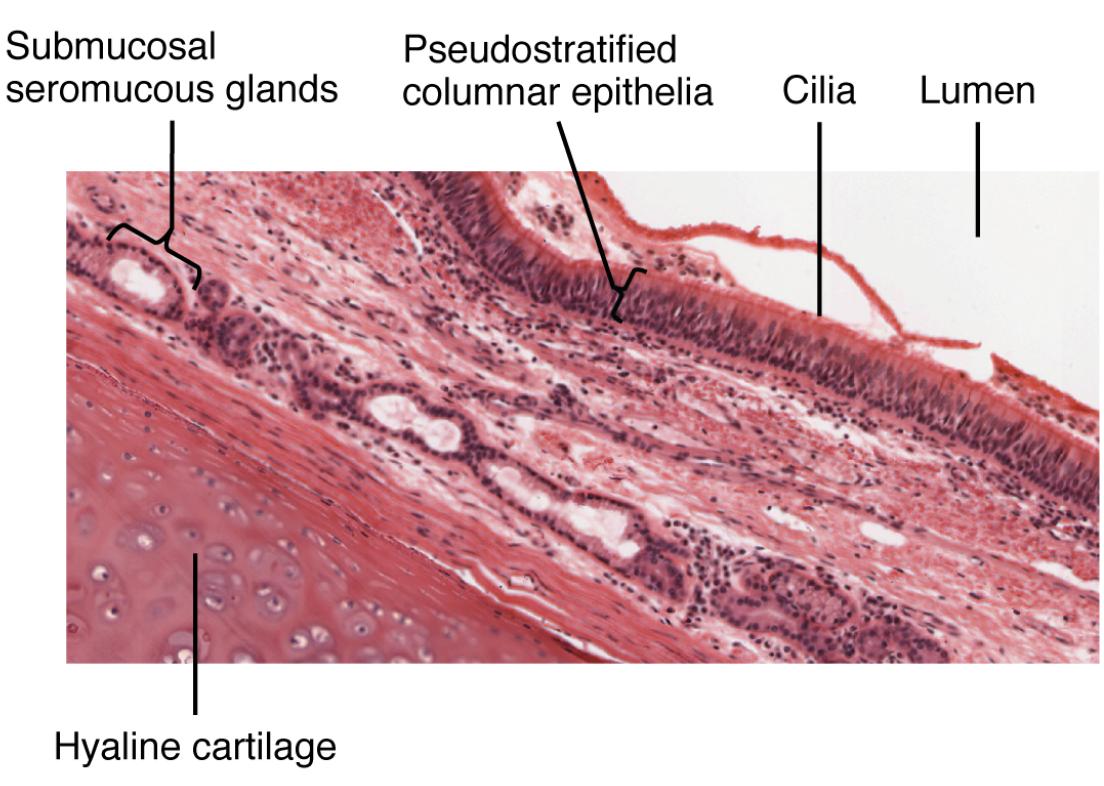
The tracheal wall, a marvel of microscopic anatomy, reveals the intricate layers that protect and maintain the airway from the hyaline cartilage to the lumen. This cross-sectional view highlights the mucosa, composed of pseudostratified ciliated columnar epithelium with goblet cells, which plays a pivotal role in filtering and humidifying air. Delving into this magnified perspective, captured at 1220x, offers a deeper understanding of the cellular mechanisms that ensure respiratory health.
Key Anatomical Labels in the Diagram
This section provides a detailed examination of each labeled component, shedding light on their functions within the tracheal wall.
Hyaline cartilage: Hyaline cartilage forms the supportive framework beneath the tracheal mucosa, providing structural rigidity to prevent collapse. Its C-shaped rings allow flexibility while maintaining an open airway for air passage.
Mucosa: The mucosa is the innermost layer visible between the hyaline cartilage and lumen, consisting of pseudostratified ciliated columnar epithelium with goblet cells. This layer traps dust and pathogens with mucus, while cilia move it upward to clear the respiratory tract.
Lumen: The lumen represents the central hollow space of the trachea, serving as the conduit for air to reach the lungs. Its patency is safeguarded by the overlying mucosal and cartilaginous layers, ensuring efficient respiration.
Submucosa: The submucosa lies beneath the mucosa, containing connective tissue, blood vessels, and glands that nourish the epithelial layer. It supports mucus production and delivers nutrients to maintain the mucosa’s protective function.
Goblet cells: Goblet cells are specialized cells within the mucosa that secrete mucus to capture inhaled particles and pathogens. Their activity complements the cilia, enhancing the airway’s filtration system.
Cilia: Cilia are microscopic hair-like structures on the mucosal epithelium that beat rhythmically to propel mucus upward. This movement, part of the mucociliary escalator, clears debris and prevents lower respiratory infections.
Microscopic Layers of the Tracheal Wall
The tracheal wall’s microscopic structure reveals a sophisticated defense system. These layers work together to optimize respiratory function.
- The mucosa’s pseudostratified epithelium maximizes surface area for air filtration.
- Goblet cells produce mucus, trapping contaminants effectively.
- Cilia move mucus upward, forming a continuous clearing mechanism.
- The submucosa nourishes the mucosa, supporting its protective role.
- Hyaline cartilage provides a stable base, preventing airway collapse.
Functional Roles in Airway Protection
The tracheal wall’s microscopic features are designed to safeguard the respiratory system. This anatomy ensures a clean and functional airway.
- The mucosa filters air, removing dust and pathogens before they reach the lungs.
- Cilia create the mucociliary escalator, expelling trapped particles.
- Goblet cells secrete mucus, humidifying air to protect delicate tissues.
- The submucosa’s blood supply sustains ciliary activity and mucus production.
- This system reduces the risk of infections like bronchitis or pneumonia.
Cellular Composition and Physiological Impact
The cellular makeup of the tracheal wall supports its respiratory duties. These components adapt to environmental challenges effectively.
- Pseudostratified ciliated columnar epithelium enhances filtration efficiency.
- Goblet cells increase mucus output in response to irritation or allergens.
- Cilia beat at a rate of 10-20 times per second, clearing mucus efficiently.
- The submucosa contains seromucous glands, releasing additional fluids.
- This cellular synergy maintains airway integrity under varying conditions.
Clinical Relevance and Anatomical Considerations
Understanding the tracheal wall’s microscopic anatomy aids in diagnosing respiratory issues. Variations can guide clinical interventions.
- Mucosal inflammation, as in tracheitis, can impair ciliary function.
- Excessive goblet cell activity may lead to chronic mucus buildup.
- Ciliary dysfunction, seen in primary ciliary dyskinesia, causes recurrent infections.
- Submucosal edema from allergies can narrow the lumen, affecting breathing.
- Microscopic analysis via biopsy helps assess these conditions accurately.
The tracheal wall’s microscopic view unveils a remarkable interplay of cartilage, mucosa, and cells that protects the airway with precision. By studying this detailed cross-section, one gains a greater appreciation for the trachea’s role in respiration, showcasing the elegance of its microscopic design.

