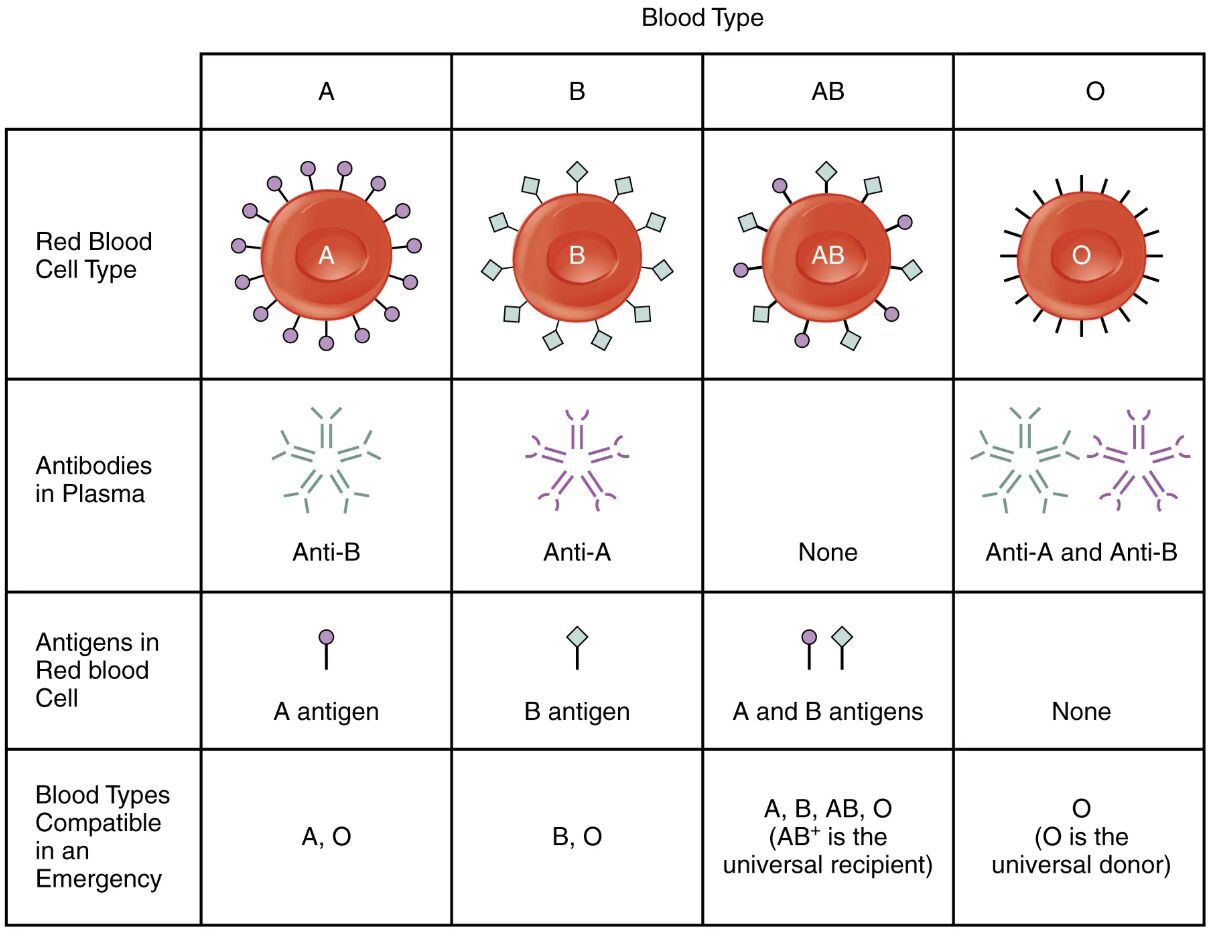
The ABO blood group system is a fundamental aspect of hematology that determines blood compatibility and transfusion safety. This article explores the characteristics of the four main blood types—A, B, AB, and O—using a detailed diagram to illustrate red blood cell antigens, plasma antibodies, and emergency compatibility. Understanding these elements is essential for navigating blood donation and transfusion practices effectively.
Red Blood Cell Type
- The red blood cell type reflects the presence of specific antigens on the surface of red blood cells, defining the blood group as A, B, AB, or O.
- These antigens are critical for determining compatibility during blood transfusions.
Antibodies in Plasma
- Antibodies in plasma are proteins that target foreign antigens, with type A blood containing Anti-B, type B containing Anti-A, type AB having none, and type O having both Anti-A and Anti-B.
- The presence or absence of these antibodies dictates the immune response to incompatible blood types.
Antigens in Red Blood Cell
- Antigens in red blood cells include the A antigen in type A, B antigen in type B, both A and B antigens in type AB, and no antigens in type O.
- These antigens trigger immune reactions if mismatched during transfusion.
Blood Types Compatible in an Emergency
- Blood types compatible in an emergency include A and O for type A, B and O for type B, A, B, AB, and O for type AB (universal recipient), and only O for type O (universal donor).
- This compatibility is crucial in urgent medical situations where immediate transfusion is required.
The ABO blood group system is a cornerstone of transfusion medicine, influencing how blood is matched and administered in clinical settings. The diagram provides a clear visual representation of the four blood types, highlighting the interplay between red blood cell antigens and plasma antibodies. This knowledge is vital for ensuring safe blood transfusions and understanding the concept of universal donors and recipients.
Blood Type A: Characteristics and Compatibility
Blood type A is defined by the presence of A antigens on red blood cells, shaping its transfusion profile. This section delves into its unique features and compatible blood types.
- Individuals with blood type A have Anti-B antibodies in their plasma, which react against B antigens.
- In emergencies, type A individuals can receive blood from type A or O donors to avoid immune reactions.
Blood Type B: Features and Transfusion Rules
Blood type B is characterized by B antigens on red blood cells, influencing its compatibility with other types. This exploration covers its antibody profile and safe donation options.
- Those with blood type B carry Anti-A antibodies, protecting against A antigen exposure.
- Emergency transfusions for type B individuals are limited to B or O blood to prevent agglutination.
Blood Type AB: The Universal Recipient
Blood type AB stands out due to the presence of both A and B antigens, earning it the title of universal recipient. This section examines its lack of antibodies and broad compatibility.
- Individuals with AB blood have no Anti-A or Anti-B antibodies, allowing them to receive any ABO blood type.
- This versatility makes AB a critical resource in complex transfusion scenarios.
Blood Type O: The Universal Donor
Blood type O is unique with no A or B antigens, designating it as the universal donor. This discussion highlights its antibody presence and donation potential.
- Type O individuals possess both Anti-A and Anti-B antibodies, restricting their receipt to O blood only.
- Its lack of antigens allows O blood to be safely transfused to all other blood types in emergencies.
The ABO blood group system classifies blood into four types—A, B, AB, and O—based on the presence or absence of A antigens and B antigens on red blood cells. These antigens are glycoproteins or glycolipids on the surface of erythrocytes, inherited from parental genes, and play a pivotal role in immune recognition. The plasma of each blood type contains corresponding antibodies: Anti-B in type A, Anti-A in type B, none in type AB, and both Anti-A and Anti-B in type O. This antibody-antigen relationship determines transfusion compatibility, as mismatched blood can lead to agglutination, where red blood cells clump together, potentially causing severe reactions or death.
Type A blood features A antigens and Anti-B antibodies, making it compatible with A and O donors. The A antigen is a result of the H antigen modified by the addition of N-acetylgalactosamine, a process governed by the ABO gene. Type B blood, with B antigens and Anti-A antibodies, is compatible with B and O donors, where the B antigen involves galactose addition to the H antigen. Type AB blood, possessing both A and B antigens without antibodies, can accept A, B, AB, or O blood, reflecting its universal recipient status due to the absence of preformed antibodies against other types.
Type O blood, lacking A and B antigens, is the universal donor, compatible with all ABO types for recipients. This is because its red blood cells do not express antigens that would trigger an immune response in other blood types. However, type O individuals have both Anti-A and Anti-B antibodies, limiting their receipt to O blood only to avoid self-agglutination. The concept of universal donor and recipient is particularly relevant in emergency medicine, where rapid access to blood is critical. For instance, O-negative blood is often the first choice in trauma cases due to its universal compatibility, while AB-positive is sought for patients requiring multiple transfusions.
The determination of blood type involves serological testing, where red blood cells are mixed with Anti-A and Anti-B antisera to observe agglutination patterns. This process, known as the forward typing method, confirms the antigen presence, while reverse typing checks plasma antibodies against known A and B cells. The Rh factor, another critical blood group system, complements the ABO system but is not depicted here; its presence (Rh⁺) or absence (Rh⁻) further refines compatibility. In practice, cross-matching is performed before transfusions to ensure no adverse reactions, especially in patients with a history of transfusions or pregnancies.
Blood type distribution varies globally, influenced by genetic and evolutionary factors. Type O is the most common worldwide, particularly in indigenous populations, while AB is the rarest. These variations affect blood bank inventories and donation drives, emphasizing the need for diverse donor pools. The immune response to mismatched blood involves the activation of complement proteins and macrophages, leading to hemolysis if untreated. Understanding these dynamics enhances the ability to manage transfusion-related complications effectively.
The ABO system also has implications beyond transfusions, such as in forensic science for identifying blood at crime scenes and in studying disease associations. For example, some research suggests a correlation between blood type and susceptibility to certain infections or cardiovascular conditions, though these links require further exploration. The diagram’s emphasis on emergency compatibility underscores its practical utility, guiding healthcare professionals in life-saving decisions.
The ABO blood group system is a fascinating blend of immunology and genetics that underpins safe medical practice. By mastering the relationships between antigens, antibodies, and compatible blood types, one can appreciate the precision required in transfusion medicine. This knowledge not only enhances clinical skills but also highlights the body’s remarkable ability to distinguish self from non-self.

