This article provides an in-depth look at the surgical repair of Atrial Septal Defect (ASD) using patch closure, as clearly depicted in the provided anatomical diagram. We will explore the nature of this common congenital heart defect, detail the principles behind its surgical correction, and discuss how restoring the integrity of the atrial septum optimizes cardiac blood flow and improves long-term cardiovascular health. This comprehensive overview aims to inform medical professionals and individuals interested in congenital heart disease management.
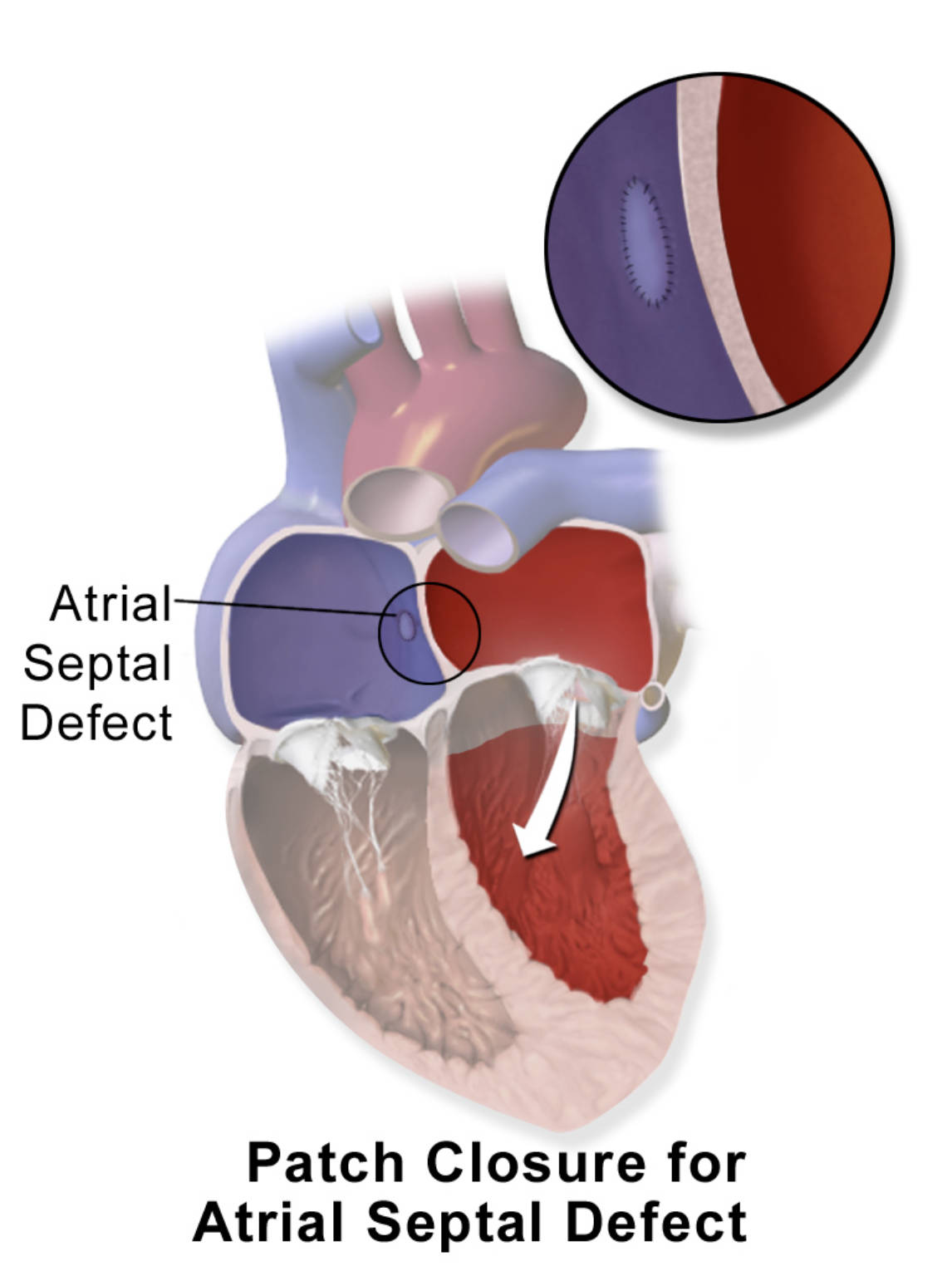
Atrial Septal Defect: This label indicates a congenital hole in the wall (septum) separating the heart’s two upper chambers, the atria. This defect allows abnormal blood flow between the left and right atria, leading to volume overload on the right side of the heart.
The diagram effectively illustrates the successful patch closure for Atrial Septal Defect, where a synthetic or biological patch has been surgically placed to cover the opening in the atrial septum. The inset provides a magnified view, showing the sutures used to secure the patch, ensuring a complete and stable repair of the defect. This intervention is crucial for restoring normal blood flow dynamics within the heart.
Atrial Septal Defect (ASD) is a type of congenital heart defect where there is an opening in the atrial septum, the wall that divides the two upper chambers of the heart (the right and left atria). This defect allows oxygenated blood from the higher-pressure left atrium to flow into the lower-pressure right atrium, a phenomenon known as a left-to-right shunt. While small ASDs may close spontaneously or remain asymptomatic, larger defects can lead to significant volume overload on the right side of the heart and the pulmonary circulation, potentially causing symptoms and complications over time. The diagram provides a clear visual of an ASD and its successful repair using a patch, showcasing a vital treatment modality.
The decision to proceed with ASD closure is typically based on the size of the defect, the presence of symptoms, and evidence of right heart enlargement or pulmonary overcirculation. Patch closure, as depicted, is a common and highly effective surgical technique used to correct larger or complex ASDs that are not suitable for catheter-based device closure. This intervention aims to eliminate the abnormal shunting of blood, thereby normalizing blood flow patterns, reducing strain on the right side of the heart, and preventing long-term complications such as pulmonary hypertension and right heart failure.
Understanding the principles of ASD repair, particularly patch closure, is essential for appreciating the advancements in treating congenital heart disease.
-
Congenital Defect: ASD is a hole in the atrial septum present at birth.
-
Left-to-Right Shunt: Oxygenated blood flows from the left atrium to the right atrium.
-
Surgical Correction: Patch closure effectively seals the defect, restoring normal hemodynamics.
These factors highlight the importance of timely and effective intervention for significant ASDs.
The Pathophysiology of Atrial Septal Defects Requiring Repair
In a healthy heart, the atrial septum ensures complete separation between the oxygenated blood in the left atrium and the deoxygenated blood in the right atrium. This prevents mixing and optimizes the efficiency of the circulatory system. However, with an Atrial Septal Defect, this separation is compromised. Due to the inherent pressure difference between the systemic circulation (left side of the heart) and the pulmonary circulation (right side of the heart), blood preferentially flows from the left atrium into the right atrium. This “left-to-right shunt” increases the volume of blood passing through the right atrium, right ventricle, and pulmonary artery.
Over time, this chronic volume overload on the right side of the heart causes the right atrium and right ventricle to dilate and work harder. The increased blood flow to the lungs, known as pulmonary overcirculation, can lead to elevated pressure in the pulmonary arteries. If left uncorrected, this can eventually cause irreversible changes in the pulmonary vasculature, resulting in pulmonary hypertension. In very advanced stages, the pulmonary pressure can become so high that the shunt reverses, leading to deoxygenated blood flowing from the right atrium to the left atrium and into the systemic circulation, a condition known as Eisenmenger syndrome, characterized by cyanosis. Surgical patch closure directly addresses this pathophysiological issue by physically sealing the defect, thereby stopping the abnormal shunting and allowing the right heart chambers and pulmonary circulation to normalize over time.
Indications and Types of ASD Closure
The decision to close an Atrial Septal Defect is typically made when there is evidence of significant left-to-right shunting, right ventricular enlargement, or clinical symptoms. These symptoms can include shortness of breath, fatigue, exercise intolerance, or recurrent respiratory infections. While small ASDs (less than 3 mm) may close spontaneously, particularly in childhood, larger defects usually require intervention.
There are two main approaches to ASD closure:
-
Catheter-based Device Closure: This minimally invasive procedure is primarily used for secundum ASDs that are centrally located and have adequate rims of tissue surrounding the defect. A specialized device, such as a septal occluder, is delivered through a catheter and deployed to close the hole without open-heart surgery.
-
Surgical Patch Closure: This involves open-heart surgery, often performed through a sternotomy or a minimally invasive approach. A patch, made from either synthetic material (e.g., Dacron) or the patient’s own pericardial tissue, is sewn directly over the defect. As shown in the diagram, the patch is meticulously sutured into place, providing a permanent seal. Surgical closure is typically chosen for larger or more complex ASDs, such as primum ASDs, sinus venosus ASDs, or when other cardiac repairs are simultaneously required.
The type of closure chosen depends on the defect’s size, location, and associated anatomical features, as well as the patient’s overall health.
Surgical Procedure and Post-Operative Outlook
Surgical patch closure for an Atrial Septal Defect is performed under general anesthesia, usually with the patient on cardiopulmonary bypass, which temporarily takes over the function of the heart and lungs. The surgeon gains access to the heart, carefully opens the right atrium, and identifies the ASD. A patch, which may be made of synthetic material like Dacron or a portion of the patient’s own pericardial tissue, is then meticulously sewn over the defect using fine sutures. The magnified inset in the diagram clearly illustrates this precise suturing of the patch, ensuring a secure and permanent repair. Once the patch is firmly in place, the heart is closed, and the patient is weaned off bypass.
The long-term prognosis after successful ASD patch closure is generally excellent. The heart’s chambers, particularly the right atrium and right ventricle, often remodel and return to a more normal size and function within several months to a year after the operation. Symptoms typically resolve, and the risk of complications like pulmonary hypertension and right heart failure significantly decreases. Most individuals can expect to lead a normal life with few, if any, restrictions. However, lifelong follow-up with a cardiologist is recommended to monitor for any residual issues, assess for potential arrhythmias, and ensure overall cardiovascular health. The success of patch closure underscores its critical role in managing congenital heart defects and improving the quality of life for affected individuals.

