Explore the innovative techniques for atrial septal defect (ASD) closure, a crucial intervention for this common congenital heart condition. This article focuses on minimally invasive device closure, a procedure that effectively repairs the defect, preventing long-term complications and improving cardiac health.
Understanding the Atrial Septal Defect Closure Diagram
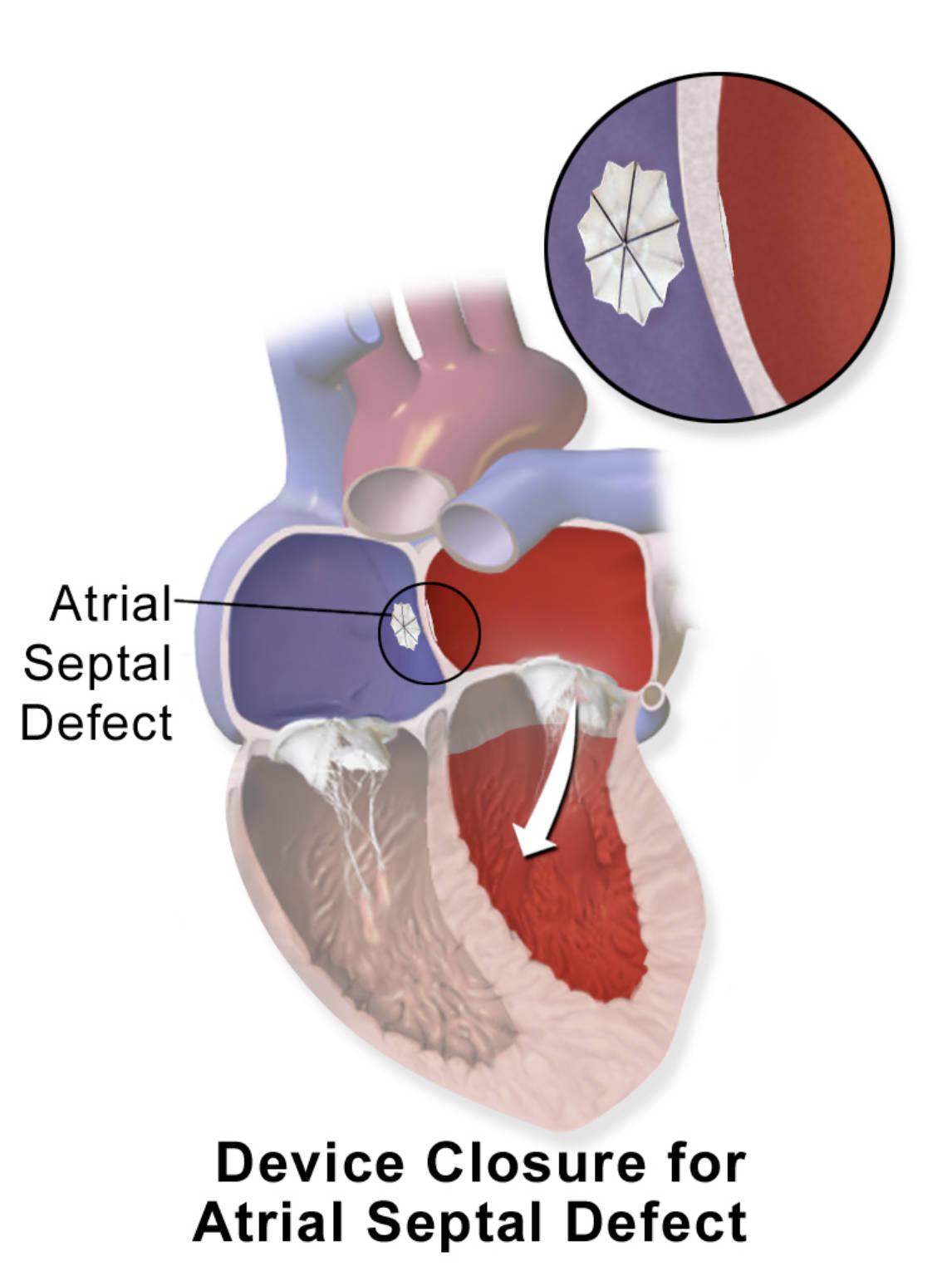
Atrial Septal Defect: This refers to a hole in the septum, the wall that separates the two upper chambers (atria) of the heart. This defect allows oxygen-rich blood from the left atrium to mix with oxygen-poor blood in the right atrium, leading to an abnormal shunting of blood.
Device (in zoomed-in view): This magnified image shows the intricate design of the occluder device used to close the atrial septal defect. It typically consists of two umbrella-like discs connected by a waist, designed to securely sandwich the septal wall around the defect.
Device Closure for Atrial Septal Defect (with arrow): This illustrates the occluder device in its final, deployed position, effectively closing the atrial septal defect. The white arrow indicates the direction of blood flow from the left atrium to the right ventricle, showing how the closure prevents the abnormal shunting.
Understanding Atrial Septal Defects
The human heart is a remarkable organ, precisely structured with four chambers separated by muscular walls, or septa, that ensure unidirectional and efficient blood flow. The interatrial septum, a wall between the two upper chambers (atria), is designed to be completely closed after birth. However, in some individuals, a congenital heart defect known as an atrial septal defect (ASD) occurs, characterized by a persistent opening in this wall. This “hole in the heart” allows oxygen-rich blood from the left atrium to shunt into the right atrium, where it mixes with oxygen-poor blood.
This abnormal shunting of blood leads to an increased volume load on the right side of the heart and the pulmonary arteries. Over time, this chronic overload can cause the right atrium and right ventricle to enlarge, and the pulmonary arteries to develop higher pressure (pulmonary hypertension). While many small ASDs may close spontaneously in infancy or remain asymptomatic into adulthood, larger defects can lead to significant complications. These can include shortness of breath, fatigue, recurrent respiratory infections, and in later life, arrhythmias (irregular heartbeats) and irreversible pulmonary vascular disease.
Historically, surgical repair of ASDs involved open-heart surgery, a highly effective but invasive procedure. However, with advancements in interventional cardiology, a less invasive approach known as transcatheter device closure has become the preferred treatment for many types of ASDs. This technique offers a safe and effective way to close the defect, preventing the long-term sequelae of chronic right-sided volume overload and significantly improving patient outcomes without the need for traditional surgery.
- Atrial septal defect (ASD) is a hole in the heart’s atrial septum.
- It causes oxygenated blood to shunt from left to right atrium.
- Large ASDs can lead to heart enlargement and pulmonary hypertension.
- Device closure is a minimally invasive repair option.
Transcatheter Device Closure Procedure
Transcatheter device closure of an atrial septal defect is a minimally invasive procedure, typically performed in a cardiac catheterization laboratory. The patient is usually under general anesthesia or conscious sedation, and the procedure involves accessing the vascular system, typically through a vein in the groin (femoral vein). A thin, flexible tube called a catheter is carefully advanced under X-ray guidance, through the venous system, and into the right side of the heart, eventually crossing the ASD into the left atrium.
Once the catheter is positioned across the defect, a specialized closure device, known as an ASD occluder, is delivered through the catheter. The most common type of device consists of two self-expanding discs made of a nickel-titanium (Nitinol) alloy mesh, connected by a central waist. One disc is deployed on the left atrial side of the septum, pulled gently against the septal wall. The second disc is then deployed on the right atrial side, effectively sandwiching the septal wall and closing the hole. The device is carefully positioned and its stability confirmed before being released from the delivery catheter.
The device is designed to become endothelialized over time, meaning that the body’s own tissue grows over the mesh, completely integrating it into the heart wall and creating a permanent seal. This process typically takes several months. The immediate effect of the closure is the elimination of the left-to-right shunt, which reduces the volume overload on the right heart and pulmonary circulation. Patients typically experience a quicker recovery compared to open-heart surgery, with shorter hospital stays and less post-procedural pain.
Indications, Risks, and Outcomes
The primary indication for ASD closure is a significant left-to-right shunt that causes right ventricular volume overload, symptoms such as exercise intolerance or fatigue, or evidence of pulmonary hypertension. The success of transcatheter device closure depends on the size, location, and anatomical features of the ASD. It is most commonly used for secundum ASDs, which are defects in the middle part of the interatrial septum. Other types of ASDs, such as primum or sinus venosus defects, often require surgical repair due to their proximity to other cardiac structures.
While generally safe and highly effective, transcatheter ASD closure carries potential risks, albeit low. These can include device embolization (the device moving from its intended position), cardiac perforation, arrhythmias, or device erosion (the device wearing through the heart tissue). Patients are typically placed on antiplatelet medication for a period after the procedure to prevent clot formation on the device. Regular follow-up, including echocardiograms, is essential to monitor the device’s position and ensure complete closure of the defect.
The long-term outcomes for patients who undergo successful ASD closure are excellent. Closure prevents or reverses the chronic volume overload on the right heart, reducing the risk of developing pulmonary hypertension, heart failure, and atrial arrhythmias in adulthood. For children, early closure can lead to normal growth and development. This minimally invasive intervention significantly improves the quality of life and long-term prognosis for individuals born with this common congenital heart condition.
Conclusion
Transcatheter device closure for atrial septal defect represents a transformative approach in the management of this prevalent congenital heart anomaly. By offering a minimally invasive, effective solution to close the “hole in the heart,” this procedure prevents progressive cardiac complications, restores normal blood flow dynamics, and significantly enhances patient well-being. The continuous advancements in interventional cardiology continue to refine such techniques, ensuring safer and more effective treatments for individuals living with congenital heart disease.

