This article provides a detailed examination of Coronary Artery Disease (CAD) by illustrating the crucial vessel changes that characterize this prevalent condition. Through a comparison of a normal artery with one experiencing narrowing due to plaque buildup, we will explore the fundamental pathology of atherosclerosis and its profound impact on cardiovascular health. This visual guide aims to enhance understanding for healthcare professionals and the general public alike, highlighting the importance of arterial health.
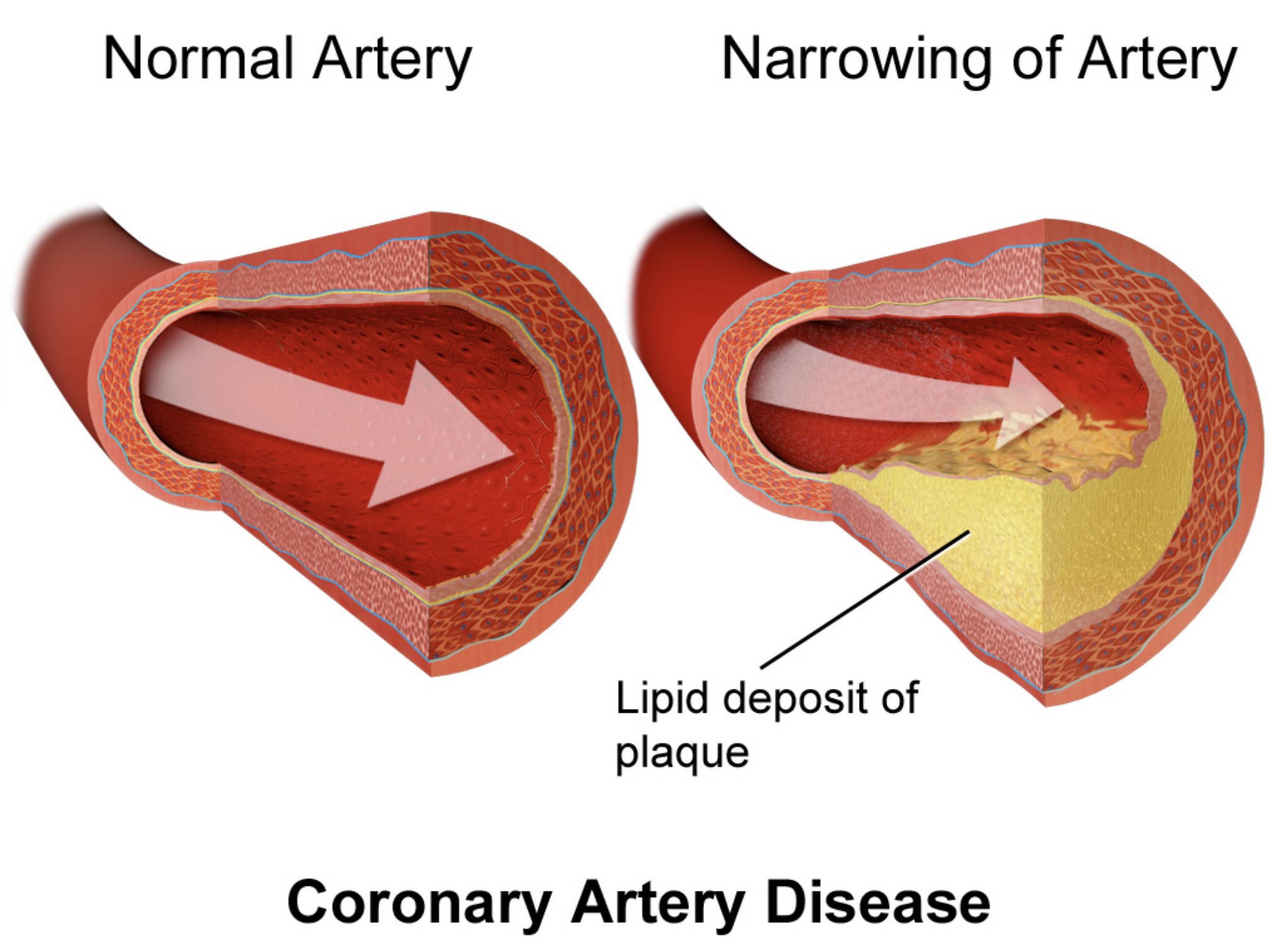
Normal Artery: This section of the diagram illustrates a healthy artery with a wide, unobstructed lumen, allowing for smooth and efficient blood flow. The inner lining is smooth, indicative of proper endothelial function, which is crucial for maintaining cardiovascular health.
Narrowing of Artery: This part of the diagram depicts an artery affected by atherosclerosis, where the lumen is significantly constricted. The narrowing is caused by the accumulation of plaque, which impedes normal blood flow and reduces the supply of oxygen and nutrients to tissues.
Lipid deposit of plaque: This label points to the yellowish material accumulating within the arterial wall, representing the atherosclerotic plaque. This deposit primarily consists of cholesterol, fatty substances, cellular waste products, and calcium, leading to the hardening and narrowing of the artery.
Coronary Artery Disease (CAD) is a significant and widespread cardiovascular condition characterized by the progressive narrowing of the coronary arteries. These vital blood vessels are responsible for supplying oxygen-rich blood to the heart muscle itself. The visual comparison provided in the diagram dramatically illustrates the core problem: a healthy artery with unimpeded blood flow versus an artery severely compromised by atherosclerotic plaque. This reduction in the arterial lumen directly impairs the delivery of essential oxygen and nutrients to the myocardium, leading to potentially life-threatening consequences.
The development of CAD is primarily driven by atherosclerosis, a chronic inflammatory disease involving the buildup of lipid deposit of plaque within the arterial walls. This process is insidious, often progressing silently for many years before symptoms become apparent. The transformation from a clear, efficient conduit to a constricted, compromised vessel is central to the pathophysiology of heart attacks, angina, and other serious cardiovascular events.
Understanding the visual difference between a normal artery and one with significant narrowing due to plaque is fundamental. This stark contrast underscores the importance of preventive measures and early intervention in managing risk factors.
- Unobstructed Blood Flow: A normal artery ensures optimal delivery of oxygen and nutrients to the heart muscle.
- Plaque Accumulation: Atherosclerotic plaque, composed of lipids and other cellular debris, progressively narrows the arterial lumen.
- Impaired Myocardial Supply: This narrowing restricts blood flow, leading to oxygen deprivation of the heart muscle, especially during periods of increased demand.
These elements collectively contribute to the development and progression of Coronary Artery Disease.
The Process of Atherosclerosis in Coronary Arteries
Atherosclerosis is a complex and progressive disease that typically begins with damage to the endothelium, the delicate inner lining of the arteries. This damage can be instigated by various factors, including high blood pressure, elevated levels of low-density lipoprotein (LDL) cholesterol, smoking, diabetes, and chronic inflammation. Once the endothelial lining is compromised, it becomes more permeable, allowing LDL cholesterol particles to penetrate into the arterial wall. These LDL particles undergo oxidation, which triggers an inflammatory response. Monocytes, a type of white blood cell, are then recruited to the site of injury, where they transform into macrophages. Macrophages engulf the oxidized LDL, becoming foam cells, which are the earliest cellular components of an atherosclerotic lesion, known as a fatty streak.
As the disease progresses, smooth muscle cells from the media (middle layer of the arterial wall) migrate to the intima (inner layer) and proliferate. These smooth muscle cells, along with macrophages, produce extracellular matrix components like collagen, contributing to the formation of a fibrous cap over the lipid-rich core. This entire structure constitutes the atherosclerotic plaque. The diagram clearly depicts this plaque encroaching into the lumen of the artery, causing significant narrowing of artery. This progressive constriction reduces the blood flow, leading to a diminished supply of oxygen and nutrients to the heart muscle. The stability of these plaques is critical; vulnerable plaques, characterized by a thin fibrous cap and a large lipid core, are prone to rupture, leading to acute thrombus formation and sudden arterial occlusion.
Clinical Impact and Diagnosis of CAD
The reduction in blood flow to the heart muscle due to narrowed coronary arteries can manifest in various clinical symptoms. The most common symptom is angina pectoris, a sensation of chest pain or discomfort that typically occurs during physical exertion or emotional stress when the heart’s demand for oxygen exceeds the supply. This pain can radiate to the arm, shoulder, back, neck, or jaw. As the narrowing becomes more severe, angina may occur even at rest, indicating unstable angina, a more serious condition. Other symptoms can include shortness of breath, fatigue, and palpitations. In some cases, particularly in women, diabetics, and the elderly, CAD can present as “silent ischemia,” where there are no noticeable symptoms despite significant arterial blockage.
Diagnosing Coronary Artery Disease involves a thorough medical history, physical examination, and a battery of diagnostic tests. An electrocardiogram (ECG) can detect abnormalities in heart rhythm and signs of heart muscle damage. Blood tests are performed to assess cholesterol levels, blood glucose, and markers of inflammation, as well as cardiac enzymes (like troponin) if a heart attack is suspected. Stress tests, which can be exercise-induced or pharmacological, help evaluate the heart’s function under increased demand and identify areas of reduced blood flow. The definitive diagnostic tool is often coronary angiography, an invasive procedure that uses contrast dye and X-rays to visualize the coronary arteries and pinpoint the exact location and severity of blockages.
Management and Prevention Strategies
Managing Coronary Artery Disease is a lifelong endeavor aimed at alleviating symptoms, preventing disease progression, and reducing the risk of cardiovascular events. The treatment approach is individualized and typically involves a combination of lifestyle modifications, pharmacological therapy, and, if necessary, revascularization procedures. Lifestyle changes are fundamental and include adopting a heart-healthy diet rich in fruits, vegetables, and whole grains; engaging in regular physical activity; maintaining a healthy weight; quitting smoking; and managing stress effectively.
Pharmacological treatments play a crucial role. Statins are prescribed to lower cholesterol levels, antiplatelet medications (e.g., aspirin) help prevent blood clots, beta-blockers reduce heart rate and blood pressure, and ACE inhibitors or angiotensin receptor blockers control blood pressure and improve cardiac function. Nitrates are often used to relieve angina symptoms. For significant blockages or when symptoms are severe despite medical therapy, revascularization may be recommended. This includes percutaneous coronary intervention (PCI), which involves using a balloon to open the artery and often placing a stent to keep it open, or coronary artery bypass grafting (CABG) surgery, which creates new pathways for blood flow around blocked arteries using grafts from other vessels. Prevention is key, and aggressive management of modifiable risk factors can significantly reduce the incidence and progression of CAD.

