Discover the life-changing technology of implanted pacemakers, essential medical devices designed to regulate abnormal heart rhythms (arrhythmias). These devices deliver precise electrical impulses to the heart, ensuring a consistent and effective heartbeat, thereby significantly improving the quality of life for patients with bradycardia and other cardiac conduction disorders.
Understanding the Implanted Pacemaker Diagram
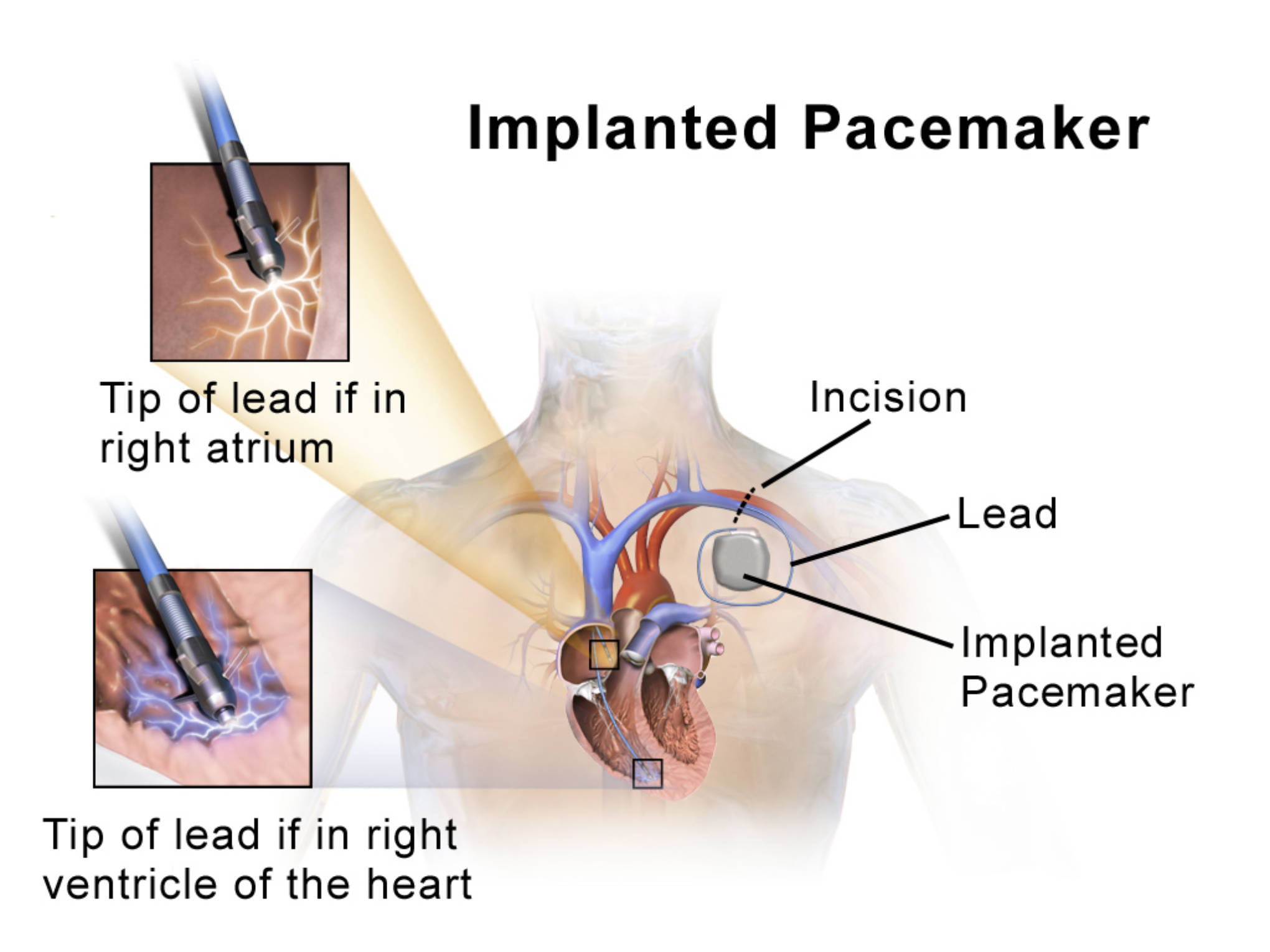
Incision: This marks the site on the chest where a small surgical cut is made, typically below the collarbone, to create a pocket for the pacemaker generator. The incision is carefully closed after the device is implanted.
Lead: These are thin, insulated wires that connect the pacemaker generator to the heart. The leads transmit electrical impulses from the generator to the heart muscle and send information about the heart’s natural electrical activity back to the generator.
Implanted Pacemaker: This refers to the pacemaker pulse generator, a small, battery-powered device containing the electronic circuitry that monitors heart rhythm and delivers electrical impulses. It is typically implanted subcutaneously (under the skin) or subpectorally (under the pectoral muscle) in the chest.
Tip of lead if in right atrium: This magnified view shows the distal end of a pacemaker lead securely positioned in the right atrium of the heart. The tip contains an electrode that can sense atrial electrical activity and deliver pacing impulses to this chamber.
Tip of lead if in right ventricle of the heart: This magnified view illustrates the tip of a pacemaker lead anchored in the right ventricle. The electrode at the tip allows for sensing ventricular activity and delivering pacing pulses to stimulate ventricular contraction.
The Heart’s Electrical Symphony and Its Disruptions
The human heart is an astonishingly resilient organ, operating as a finely tuned pump whose rhythmic contractions are orchestrated by its own intrinsic electrical system. This natural pacemaker, the sinoatrial (SA) node, generates electrical impulses that spread through the atria and then to the ventricles, ensuring a coordinated and efficient heartbeat. This intricate electrical symphony is responsible for circulating blood throughout the body, delivering oxygen and nutrients to every cell.
However, various medical conditions can disrupt this delicate electrical rhythm, leading to arrhythmias. One common type of arrhythmia that often necessitates pacemaker implantation is bradycardia, a condition where the heart beats too slowly. This can be due to a malfunctioning SA node (sick sinus syndrome) or a block in the electrical pathways between the atria and ventricles (heart block). When the heart rate is persistently too slow, it can lead to insufficient blood flow to the body, causing symptoms such as fatigue, dizziness, shortness of breath, and fainting spells (syncope).
For individuals experiencing symptomatic bradycardia or other conduction disorders that compromise cardiac output, an implanted pacemaker offers a life-changing solution. These sophisticated devices are designed to continuously monitor the heart’s natural electrical activity and intervene only when necessary, delivering precisely timed electrical impulses to stimulate the heart muscle. By ensuring a consistent and appropriate heart rate, pacemakers restore normal cardiac function, alleviate debilitating symptoms, and significantly improve a patient’s quality of life and longevity.
-
The heart’s electrical system dictates its rhythm.
-
Bradycardia is a common reason for pacemaker implantation.
-
Pacemakers regulate slow heart rhythms.
-
They deliver electrical impulses to the heart.
Components and Function of an Implanted Pacemaker
An implanted pacemaker system typically consists of two main components: the pulse generator and one or more leads (or electrodes). The pulse generator is a small, hermetically sealed device containing a long-lasting battery and sophisticated electronic circuitry. This circuitry is programmed to detect the heart’s natural electrical activity. If the heart rate falls below a programmed threshold, or if certain electrical events fail to occur (e.g., a signal from the atrium to the ventricle), the generator delivers a tiny electrical impulse through the leads to stimulate the heart muscle.
The leads are thin, insulated wires made of biocompatible materials that are threaded through a vein, typically in the subclavian region, into the chambers of the heart. The distal tips of the leads contain electrodes that make direct contact with the heart muscle, usually in the right atrium and/or right ventricle. These electrodes serve a dual purpose: they “sense” the heart’s intrinsic electrical activity and “pace” the heart by delivering electrical impulses when needed. Depending on the specific arrhythmia and the patient’s needs, a pacemaker might have one lead (single-chamber), two leads (dual-chamber), or even three leads for biventricular pacing in cases of heart failure.
Pacemakers are highly programmable and can be adjusted non-invasively by a cardiologist using an external programmer. Modern pacemakers feature advanced sensing capabilities, allowing them to adapt their pacing rate to the patient’s activity level (rate-responsive pacemakers). This ensures that the heart rate increases during physical exertion and slows down during rest, mimicking the body’s natural physiological response. The battery life of a pacemaker typically ranges from 5 to 15 years, after which the pulse generator needs to be replaced in a minor surgical procedure.
Implantation Procedure and Living with a Pacemaker
The implantation of a pacemaker is a relatively routine surgical procedure, usually performed under local anesthesia with sedation. An incision is made in the upper chest, typically just below the collarbone, to create a small pocket for the pulse generator. The pacemaker leads are then carefully guided through a vein into the appropriate heart chambers under X-ray guidance. Once correctly positioned, the lead tips are secured to the heart muscle, and the other ends are connected to the pulse generator. The generator is then placed in its subcutaneous pocket, and the incision is closed.
Living with an implanted pacemaker generally involves few restrictions. Patients are usually advised to avoid strong magnetic fields, which can interfere with the device’s function, though most common household appliances are safe. Regular follow-up appointments with a cardiologist are essential to monitor the pacemaker’s function, check battery life, and adjust programming as needed. While a pacemaker significantly improves the symptoms of bradycardia and can be life-saving, it does not cure the underlying heart condition. However, it allows patients to lead active and fulfilling lives, free from the debilitating effects of a slow or irregular heartbeat.
Conclusion
Implanted pacemakers stand as a cornerstone of modern cardiology, offering a highly effective and safe treatment for a range of cardiac rhythm disorders. By meticulously monitoring and regulating the heart’s electrical activity, these devices ensure a consistent and appropriate heartbeat, thereby restoring normal physiological function and significantly enhancing patient well-being. The continuous advancements in pacemaker technology underscore their profound impact on improving cardiac health and extending the lives of individuals challenged by an unreliable natural pacemaker.

