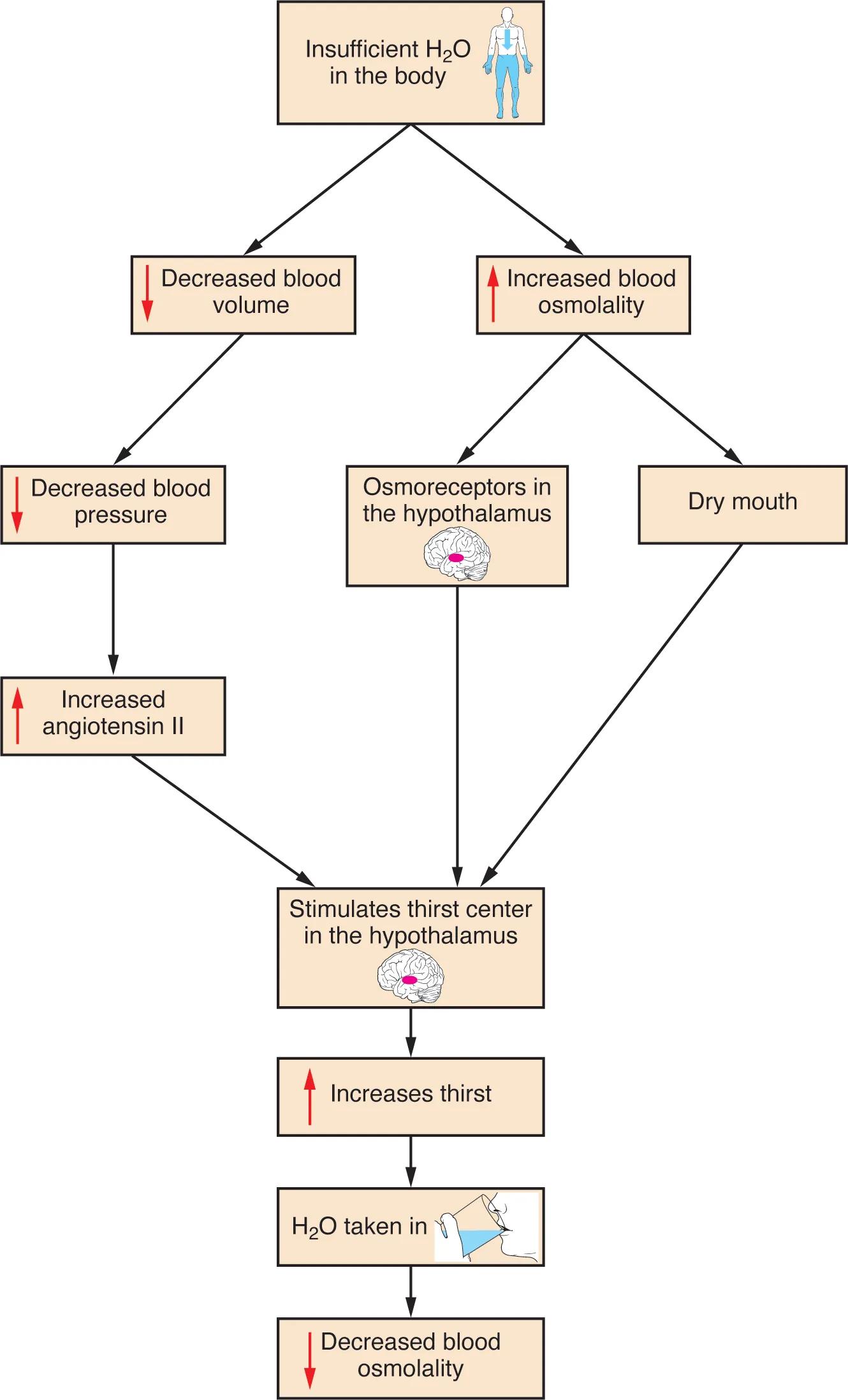
Insufficient water in the body triggers a complex and vital physiological response to restore fluid balance. This flowchart illustrates the intricate mechanisms by which the body detects dehydration and stimulates thirst, ultimately leading to increased water intake and the re-establishment of optimal blood osmolality. Understanding this pathway is crucial for comprehending the body’s homeostatic control over hydration.
Understanding the Thirst Response
Insufficient H2O in the body: This initial state signifies a lack of adequate water in the body, which can arise from various factors such as inadequate fluid intake, excessive sweating, or certain medical conditions. This deficiency sets off a cascade of physiological events aimed at correcting the imbalance.
Decreased blood volume: When there is insufficient water in the body, the total volume of blood circulating within the cardiovascular system decreases. This reduction in blood volume directly impacts blood pressure and overall circulatory efficiency.
Increased blood osmolality: Insufficient H2O in the body leads to a higher concentration of solutes (like salts and proteins) in the blood relative to water, resulting in increased blood osmolality. This change in concentration is a key signal for the body’s hydration sensors.
Decreased blood pressure: A direct consequence of decreased blood volume is a drop in blood pressure. The heart has less fluid to pump, which reduces the force exerted against the arterial walls.
Osmoreceptors in the hypothalamus: Located in the hypothalamus, a crucial part of the brain, these specialized sensory receptors are highly sensitive to changes in blood osmolality. When blood osmolality increases, these osmoreceptors detect the change and send signals to initiate the thirst response. The hypothalamus plays a central role in regulating many bodily functions, including fluid balance.
Dry mouth: Reduced saliva production due to dehydration leads to a sensation of dry mouth. This physical discomfort is a direct and immediate signal that contributes to the overall feeling of thirst.
Increased angiotensin II: A decrease in blood pressure triggers a series of hormonal responses, including an increase in angiotensin II. This potent hormone plays a vital role in regulating blood pressure and fluid balance, and it also directly stimulates the thirst center.
Stimulates thirst center in the hypothalamus: Various signals converge on the thirst center, also located in the hypothalamus. These signals include input from osmoreceptors, dry mouth sensations, and increased angiotensin II levels. The thirst center integrates these signals to generate the sensation of thirst.
Increases thirst: The stimulation of the thirst center results in a conscious feeling of thirst, prompting an individual to seek out and consume fluids. This is the behavioral component of the thirst response.
H2O taken in: This step represents the voluntary action of drinking water in response to increased thirst. It is the crucial behavioral intervention that begins to correct the body’s fluid imbalance.
Decreased blood osmolality: As water is taken in and absorbed, it dilutes the concentration of solutes in the blood, thereby decreasing blood osmolality. This restoration of normal osmolality signals the body that sufficient water has been consumed, helping to satiate thirst.
The Body’s Intricate Hydration System
The body’s regulation of water balance is a finely tuned example of homeostasis, essential for maintaining physiological functions. The thirst response, as depicted in this flowchart, is a primary mechanism to prevent dehydration and ensure proper cellular function. When the body experiences a deficit of water, whether due to insufficient intake or increased loss, two critical changes occur: a decrease in blood volume and an increase in blood osmolality. Both of these changes act as potent stimuli to initiate the thirst cascade.
The hypothalamus, a small but vital region of the brain, serves as the central processing unit for these signals. It houses osmoreceptors that directly monitor blood osmolality, and it also contains the thirst center, which integrates various inputs. For instance, a decrease in blood pressure, a direct consequence of reduced blood volume, triggers the release of hormones like angiotensin II, further stimulating the thirst center. Simultaneously, the uncomfortable sensation of a dry mouth provides another powerful cue, contributing to the overall drive to drink.
These converging signals culminate in the sensation of thirst, motivating an individual to consume water. This behavioral response is critical. Once water is ingested, it is absorbed into the bloodstream, which then dilutes the concentrated solutes, thereby decreasing blood osmolality and increasing blood volume. This process then reduces the initial stimuli, completing the feedback loop and restoring the body’s fluid balance. Understanding this intricate interplay of physiological and behavioral responses provides insight into the body’s remarkable ability to self-regulate and maintain internal stability.
Restoring Fluid Balance
Maintaining adequate hydration is paramount for overall health, as water plays a critical role in nutrient transport, waste elimination, temperature regulation, and joint lubrication. Disruptions in the thirst response, or chronic insufficient water intake, can lead to dehydration, manifesting in symptoms ranging from mild fatigue and dizziness to severe physiological disturbances. Therefore, recognizing the signs of thirst and responding to them promptly is a fundamental aspect of self-care. This diagram serves as an excellent visual aid for anyone seeking to understand the fundamental physiological processes underpinning one of our most basic and essential needs.
The Thirst Response: A Vital Homeostatic Mechanism
The human body is an intricate network of systems, each working in concert to maintain a stable internal environment, a concept known as homeostasis. One of the most critical aspects of this balance is the regulation of fluid levels, specifically water. The thirst response, as detailed in the accompanying flowchart, is a sophisticated and highly effective homeostatic mechanism designed to prevent and correct dehydration. This process begins with the detection of insufficient H2O in the body, a state that can arise from various factors such as physical activity, warm climates, or simply not drinking enough fluids.
When water levels drop, the body experiences two primary physiological changes: a decreased blood volume and an increased blood osmolality. The reduction in blood volume directly leads to a decrease in blood pressure, triggering a cascade that includes the release of angiotensin II, a powerful vasoconstrictor that also stimulates the thirst center. Concurrently, the increased concentration of solutes in the blood (higher osmolality) is detected by specialized osmoreceptors located in the hypothalamus, a key region of the brain responsible for regulating many bodily functions, including fluid balance.
Beyond these internal sensors, a more immediate and noticeable signal is the sensation of a dry mouth, caused by reduced saliva production. All these signals—from the osmoreceptors, angiotensin II, and dry mouth—converge on the thirst center, also situated in the hypothalamus. The integration of these various inputs generates the powerful urge to drink, leading to increased thirst. The act of H2O taken in then initiates the corrective phase. As water is absorbed into the bloodstream, it dilutes the concentrated solutes, thereby decreasing blood osmolality, and restores blood volume, ultimately alleviating the initial stimuli and bringing the body back into a state of optimal hydration. This intricate feedback loop ensures that the body’s water levels are meticulously maintained, highlighting the elegance and efficiency of our physiological regulatory systems.

