The heart’s rhythm is a dynamic process influenced by the autonomic nervous system, which adjusts heart rate to meet the body’s changing needs. This regulation is depicted through the effects of parasympathetic stimulation and sympathetic stimulation on the normal sinus rhythm, showcasing how the heart adapts to rest or activity. Understanding these mechanisms offers valuable insights into cardiovascular function and the balance required for optimal health.
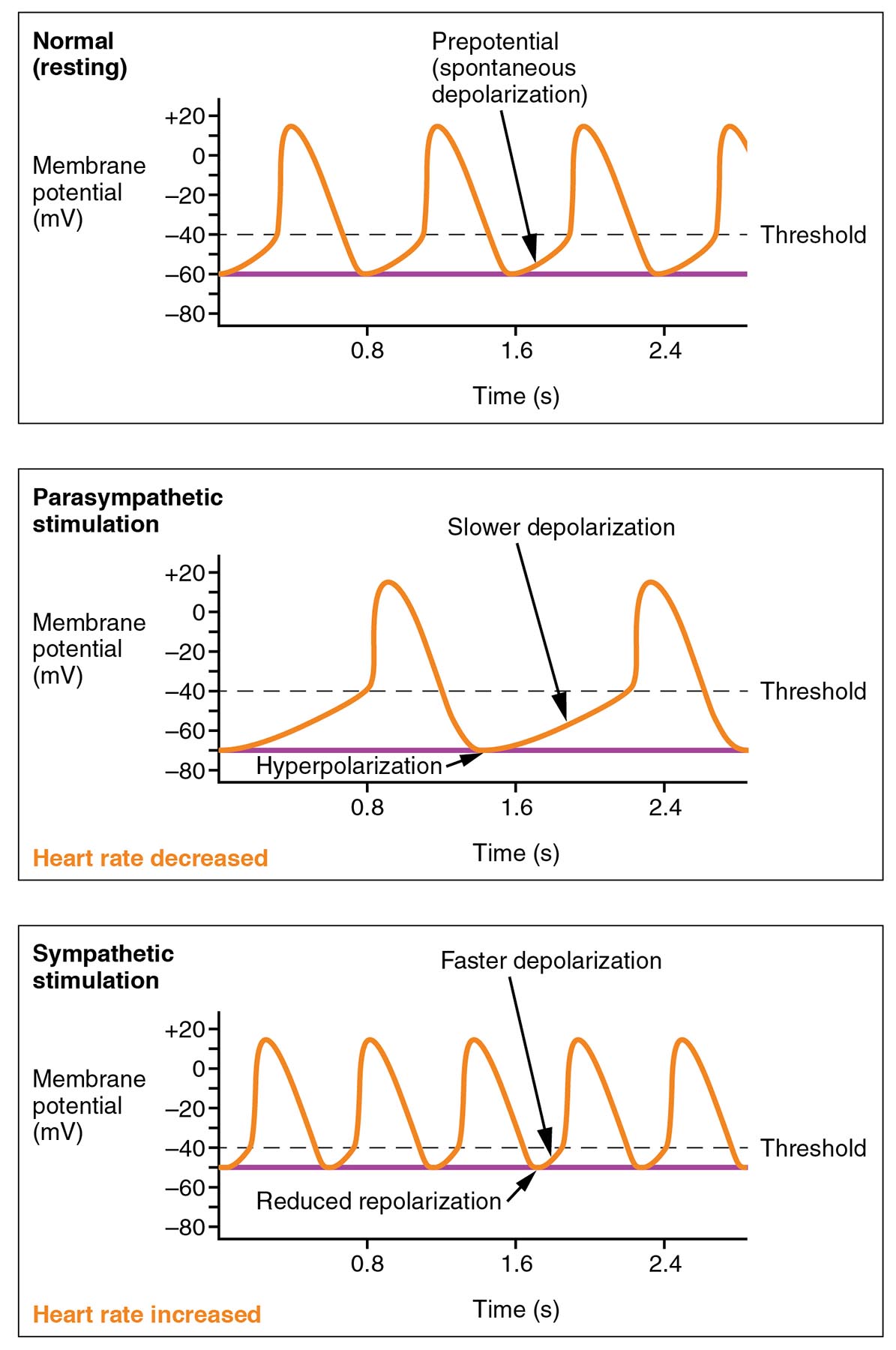
Normal (resting) Normal (resting) represents the baseline membrane potential and spontaneous depolarization of the sinoatrial node under typical conditions. The wave pattern shows a steady heart rate, with the threshold reached at regular intervals of approximately 0.8 to 2.4 seconds.
Prepotential (spontaneous depolarization) Prepotential (spontaneous depolarization) is the gradual rise in membrane potential leading to the action potential in pacemaker cells. This phase, driven by funny currents and calcium influx, determines the inherent rhythm of the heart at rest.
Threshold Threshold is the critical membrane potential level, around -40 mV, where an action potential is triggered in the sinoatrial node. Reaching this point initiates the rapid depolarization phase, setting the pace for each heartbeat.
Parasympathetic stimulation Parasympathetic stimulation involves vagus nerve activity that slows heart rate by hyperpolarizing the membrane, delaying the time to reach the threshold. This results in a slower depolarization slope, as seen with an extended interval between beats.
Slower depolarization Slower depolarization occurs under parasympathetic influence, reducing the rate of membrane potential rise toward the threshold. This effect lengthens the cardiac cycle, contributing to a decreased heart rate during rest or recovery.
Hyperpolarization Hyperpolarization is the increased negativity of the membrane potential following parasympathetic stimulation, pushing it below the resting level. This shift delays the onset of the next action potential, further slowing the heart rate.
Heart rate decreased Heart rate decreased is the net outcome of parasympathetic stimulation, reflected by longer intervals between action potentials. This reduction helps conserve energy and supports cardiovascular stability during low-demand states.
Sympathetic stimulation Sympathetic stimulation activates the sympathetic nervous system, accelerating heart rate through faster depolarization and reduced repolarization time. This response is mediated by norepinephrine, enhancing cardiac output during stress or exercise.
Faster depolarization Faster depolarization under sympathetic influence quickens the rise of membrane potential toward the threshold, shortening the time between beats. This rapid phase ensures the heart can meet increased metabolic demands efficiently.
Reduced repolarization Reduced repolarization occurs as sympathetic stimulation shortens the recovery phase, allowing quicker preparation for the next action potential. This adjustment supports a higher heart rate by minimizing the interval between cycles.
Heart rate increased Heart rate increased is the result of sympathetic stimulation, evident in the shortened cycle length and more frequent threshold crossings. This elevation prepares the body for physical activity or acute stress responses.
Fundamentals of Heart Rate Regulation
Heart rate regulation is a finely tuned process governed by the autonomic nervous system. It ensures the heart adapts to varying physiological conditions seamlessly.
- The normal (resting) state reflects the intrinsic pacemaker activity of the sinoatrial node.
- Parasympathetic stimulation via the vagus nerve slows this rhythm for energy conservation.
- Sympathetic stimulation accelerates the pace to support increased demand.
- Membrane potential changes are driven by ion movements, including sodium and potassium.
- Hormones like adrenaline amplify these autonomic effects during emergencies.
Parasympathetic Effects on Sinus Rhythm
Parasympathetic stimulation plays a key role in calming the heart, promoting a slower rhythm. This mechanism is vital for maintaining cardiovascular health during rest.
- The vagus nerve releases acetylcholine, enhancing hyperpolarization.
- Slower depolarization extends the time to reach the threshold, reducing heart rate.
- This action lowers oxygen consumption by the heart muscle.
- Heart rate decreased supports recovery after exertion or stress.
- Baroreceptors trigger this response to manage blood pressure elevations.
Mechanisms Behind Slowed Depolarization
The process of slower depolarization involves specific ionic changes. These alterations ensure the heart operates efficiently at a reduced pace.
- Acetylcholine increases potassium efflux, causing hyperpolarization.
- This delays the funny current activation that drives prepotential (spontaneous depolarization).
- The threshold is reached more gradually, lengthening the cycle.
- Reduced calcium influx contributes to the slower pace.
- Chronic parasympathetic dominance may influence long-term heart rate trends.
Sympathetic Influence on Heart Rate
Sympathetic stimulation enhances heart rate to meet heightened physiological needs. This response is critical during physical activity or stress.
- Norepinephrine binds to beta-adrenergic receptors, speeding faster depolarization.
- Reduced repolarization shortens the recovery phase, increasing cycle frequency.
- This leads to an heart rate increased state, boosting cardiac output.
- Sympathetic nerves enhance calcium entry, strengthening contractions.
- Thyroid hormones T3 and T4 can potentiate this effect over time.
Dynamics of Faster Depolarization
Faster depolarization reflects the heart’s ability to adapt quickly. This process ensures adequate blood supply during demanding situations.
- Sodium channels open more rapidly, accelerating the rise to threshold.
- Reduced repolarization is due to decreased potassium outflow.
- The prepotential (spontaneous depolarization) slope steepens under sympathetic drive.
- This mechanism supports the heart rate increased response effectively.
- Overactivation can strain the heart if not balanced by parasympathetic input.
Clinical Significance of Autonomic Modulation
Understanding these effects aids in assessing and managing heart function. This knowledge is essential for addressing rhythm irregularities.
- Parasympathetic stimulation dysfunction may lead to tachycardia if unchecked.
- Sympathetic stimulation overactivity is linked to arrhythmias or hypertension.
- Monitoring heart rate increased or heart rate decreased guides treatment.
- Drugs like beta-blockers target sympathetic stimulation to normalize rate.
- Exercise stress tests evaluate autonomic responsiveness in healthy individuals.
In conclusion, the interplay of parasympathetic stimulation and sympathetic stimulation on the normal sinus rhythm illustrates the heart’s remarkable adaptability. These mechanisms ensure the cardiovascular system responds appropriately to rest, exercise, and stress, maintaining vital circulation. Exploring this balance deepens our appreciation of heart physiology and supports efforts to optimize cardiovascular health.

