Vascular bypass grafting is a critical surgical intervention designed to redirect blood flow around a section of a blocked or partially blocked artery in the leg. This procedure acts as a biological detour, ensuring that oxygen-rich blood can bypass an obstruction caused by atherosclerosis to reach the lower leg and foot. By restoring proper circulation, this surgery plays a vital role in limb preservation and symptom relief for patients suffering from advanced stages of arterial disease.
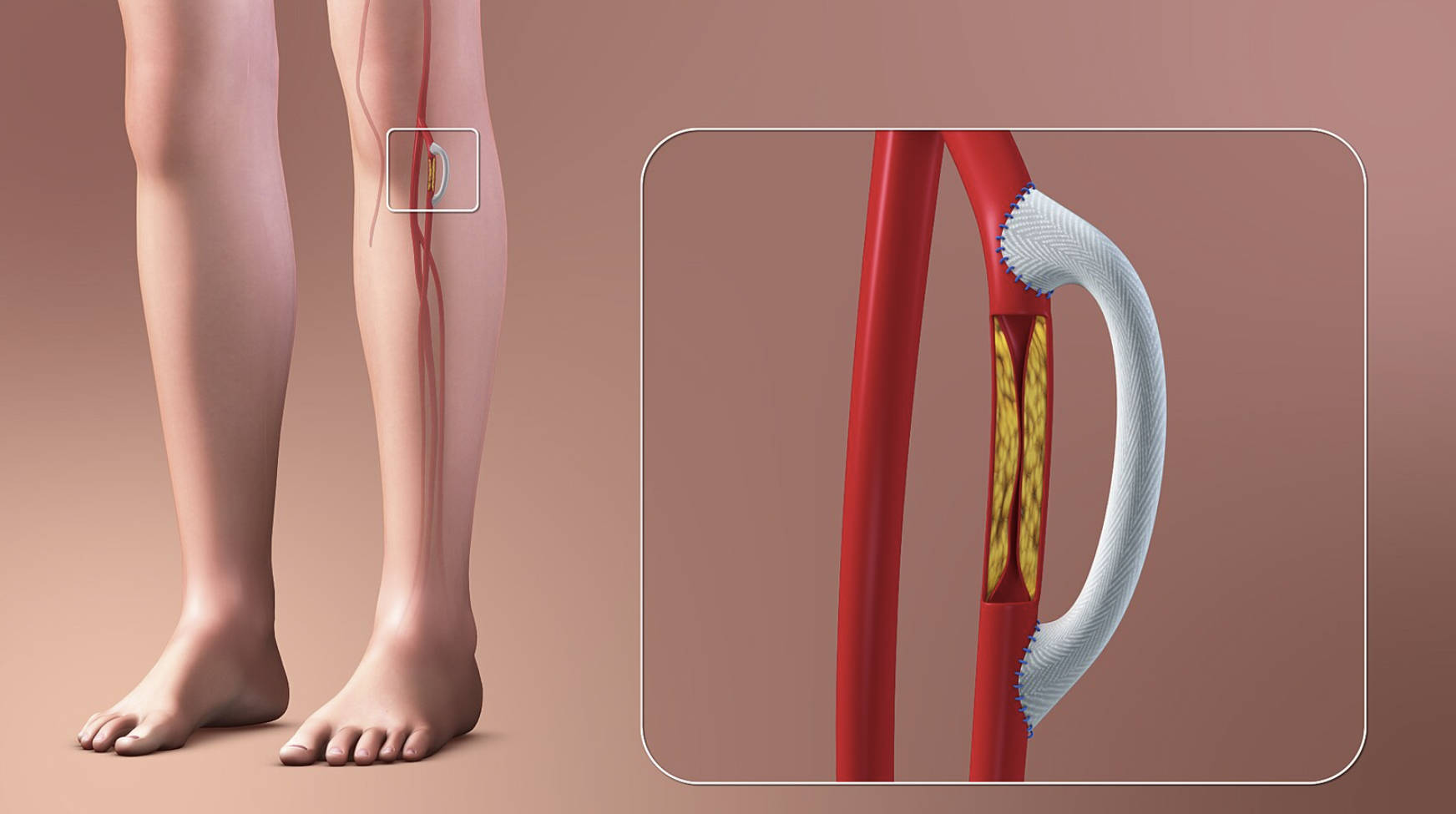
Diseased Artery: The red vessel illustrated in the background represents the native femoral or popliteal artery that has been compromised. In a healthy state, this vessel would have a smooth interior lumen, but here it serves as the site of obstruction that necessitates surgical bypass.
Atherosclerotic Plaque: The yellow substance depicted inside the cut-away section of the artery is the buildup of plaque, consisting of cholesterol, calcium, and fibrous tissue. This accumulation narrows the artery (stenosis) or blocks it completely (occlusion), physically preventing blood from flowing through the natural pathway.
Vascular Graft: The white, textured tube shown looping over the blockage is the prosthetic graft. While surgeons often use the patient’s own vein (autograft), this illustration depicts a synthetic graft, typically made from materials like Dacron or PTFE, used to create the new channel for blood flow.
Anastomosis: The blue sutures visible at the top and bottom of the white graft mark the anastomosis sites. These are the precise surgical connections where the graft is sewn into the healthy part of the artery above and below the blockage to ensure a leak-proof seal.
Understanding Lower Extremity Bypass Surgery
Peripheral vascular bypass surgery is an established procedure used to treat severe cases of arterial insufficiency. The concept is mechanically similar to a highway detour: when the main road (the artery) is blocked by debris (plaque), traffic (blood) is rerouted through a new road (the graft) to reach its destination. This restoration of perfusion is essential for the metabolic health of the muscle and skin tissues in the lower leg.
The procedure is most commonly performed to address complications arising from atherosclerosis, a systemic condition where arteries harden and narrow over time. In the lower limbs, this narrowing restricts blood supply, leading to a spectrum of symptoms ranging from mild pain during exercise to severe tissue death. When less invasive treatments, such as angioplasty or stenting, are insufficient or technically unfeasible, open bypass surgery becomes the gold standard for revascularization.
Surgeons carefully select the type of graft based on the patient’s anatomy and the location of the blockage. The “Fem-Pop” (femoral-popliteal) bypass is the most frequent, bridging the femoral artery in the thigh to the popliteal artery behind the knee. The success of the surgery depends heavily on the quality of the patient’s vessels and their overall cardiovascular health.
Common indications for recommending this surgery include:
- Critical Limb Ischemia: Severe pain in the foot or toes even while resting.
- Non-healing Wounds: Ulcers or sores on the feet or legs that persist due to poor blood flow.
- Gangrene: Tissue death that could lead to amputation if blood flow is not restored.
- Lifestyle-Limiting Claudication: Severe leg pain during walking that prevents daily activities and does not respond to medication or exercise.
Peripheral Artery Disease: Pathology and Progression
The underlying condition necessitating this surgery is Peripheral Artery Disease (PAD). PAD is a progressive circulatory problem where narrowed arteries reduce blood flow to the limbs. The pathophysiology begins with endothelial injury—damage to the inner lining of the artery caused by factors such as smoking, high blood pressure, or high blood sugar. This injury triggers an inflammatory response, leading to the deposition of lipids and the formation of the yellow plaque seen in the illustration.
As the plaque grows, the arterial lumen narrows. Initially, the body may try to compensate by developing small collateral vessels, but these are rarely sufficient to meet the metabolic demands of the leg muscles during exercise. This leads to the hallmark symptom of intermittent claudication—cramping pain in the calves or thighs that occurs with walking and resolves with rest. Without management, the plaque can rupture or become large enough to completely occlude the vessel, cutting off the nutrient supply to the foot.
In advanced stages, the lack of blood flow compromises the skin’s ability to heal and the nerves’ ability to function. Patients may experience numbness, coldness in the leg, or changes in skin color. If vascular bypass grafting is not performed in time for severe cases, the tissue starvation can progress to necrosis, necessitating amputation. Therefore, managing risk factors such as diabetes mellitus, hypertension, and hyperlipidemia is crucial for preventing the disease’s progression and ensuring the longevity of the surgical graft.
Conclusion
Vascular bypass grafting remains a limb-saving procedure for patients facing the severe consequences of arterial blockage. By creating a new pathway for blood flow, surgeons can alleviate debilitating pain, heal chronic wounds, and improve the overall quality of life. Understanding the anatomical mechanics of this surgery—how the graft bridges the atherosclerosis to restore distal perfusion—highlights the sophistication of modern vascular medicine in combating the effects of chronic disease.

