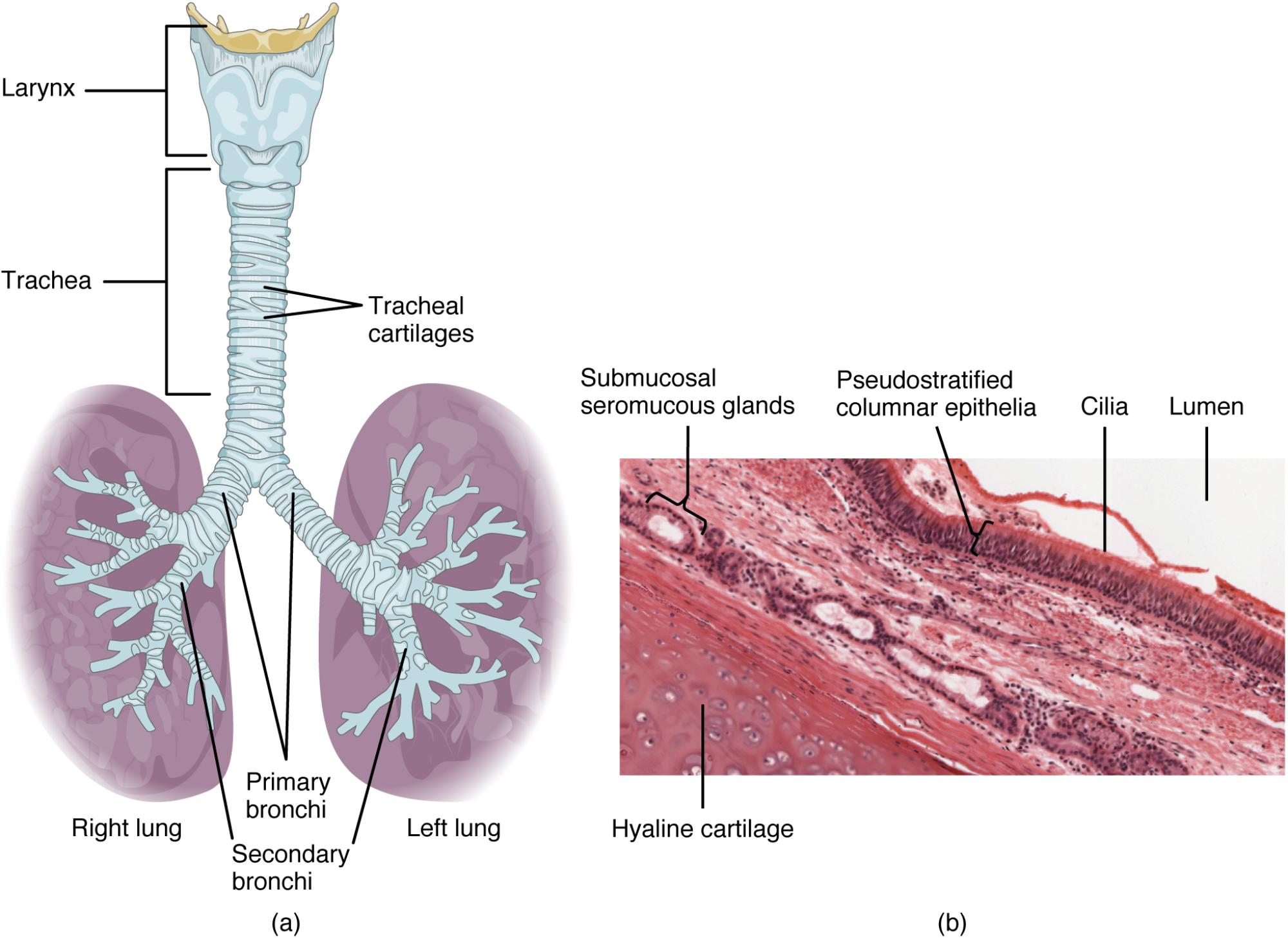
The trachea, a vital conduit for air travel from the larynx to the lungs, showcases a remarkable design with its stacked C-shaped hyaline cartilage rings. This structure, visible in both macroscopic and microscopic views, ensures airway patency while its mucosal lining, composed of pseudostratified ciliated columnar epithelium with goblet cells, filters and humidifies inhaled air. Exploring these detailed perspectives reveals the trachea’s critical role in respiration and its intricate cellular composition, offering a deeper appreciation of its functionality.
Key Anatomical Labels in the Diagram
This section outlines each labeled component, providing insights into their structure and purpose within the tracheal system.
Hyaline cartilage: Hyaline cartilage forms the C-shaped rings that provide structural support to the trachea, preventing its collapse during respiration. These rings are stacked and connected by fibrous tissue, allowing flexibility while maintaining an open airway.
Mucosa: The mucosa lines the inner tracheal wall, consisting of pseudostratified ciliated columnar epithelium with goblet cells that secrete mucus. This layer traps dust and pathogens, with cilia moving mucus upward to clear the airway.
Lumen: The lumen is the hollow central cavity of the trachea, serving as the passageway for air to travel to the lungs. Its patency is maintained by the supporting cartilage rings, ensuring efficient respiration.
Submucosa: The submucosa lies beneath the mucosa, containing connective tissue, blood vessels, and glands that nourish the tracheal wall. It supports the mucosa and aids in mucus production and immune response.
Adventitia: The adventitia is the outermost connective tissue layer of the trachea, anchoring it to surrounding structures. It provides additional stability and houses blood vessels and nerves.
Smooth muscle: Smooth muscle connects the open ends of the C-shaped cartilage rings, allowing the trachea to adjust its diameter during breathing. This muscle also aids in expelling mucus through coughing.
Goblet cells: Goblet cells are specialized cells within the mucosa that produce and secrete mucus to trap inhaled particles. Their activity is enhanced by the ciliated epithelium, which moves mucus toward the pharynx.
Cilia: Cilia are hair-like projections on the mucosal epithelium that beat rhythmically to move mucus and trapped particles upward. This mechanism, known as the mucociliary escalator, protects the lower respiratory tract.
Macroscopic Structure of the Trachea
The trachea’s external anatomy relies on its cartilage framework for strength. This design ensures a stable airway under varying conditions.
- The hyaline cartilage rings prevent collapse, especially during forced exhalation.
- The C-shape allows esophageal expansion during swallowing.
- Smooth muscle adjusts the tracheal diameter, aiding airflow regulation.
- The adventitia anchors the trachea, integrating it with the neck’s anatomy.
- This structure supports continuous air delivery to the lungs.
Microscopic Composition and Function
The tracheal wall’s microscopic view reveals a complex layering that enhances respiratory health. These layers work together to maintain a clean airway.
- The mucosa’s pseudostratified epithelium maximizes surface area for filtration.
- Goblet cells secrete mucus, trapping pathogens and debris effectively.
- Cilia beat in coordinated waves, propelling mucus upward for clearance.
- The submucosa nourishes the mucosa, supporting its protective role.
- This microscopic system prevents infections in the lower airways.
Physiological Roles in Respiration
The trachea plays a critical role in preparing air for the lungs. Its anatomy supports efficient gas exchange and protection.
- The lumen ensures a clear path for air, humidified by mucosal secretions.
- Hyaline cartilage maintains structural integrity under pressure changes.
- The mucociliary escalator removes contaminants, reducing infection risk.
- Smooth muscle contraction aids in coughing to clear blockages.
- Blood vessels in the submucosa deliver oxygen to support ciliary action.
Clinical Relevance and Anatomical Insights
Understanding tracheal anatomy aids in diagnosing and managing respiratory conditions. Variations can influence treatment strategies.
- Tracheal stenosis, from cartilage malformation, can obstruct airflow.
- Excessive mucus production by goblet cells may signal chronic bronchitis.
- Ciliary dysfunction, as in primary ciliary dyskinesia, impairs clearance.
- Trauma to the adventitia can lead to tracheal collapse or infection.
- Imaging and biopsy assess these structures for accurate diagnosis.
The trachea’s elegant combination of macroscopic support and microscopic filtration underscores its importance in respiration. By examining its anatomical structure and cellular details through these views, one gains a profound understanding of its role in maintaining lung health, highlighting the sophistication of this essential airway.

