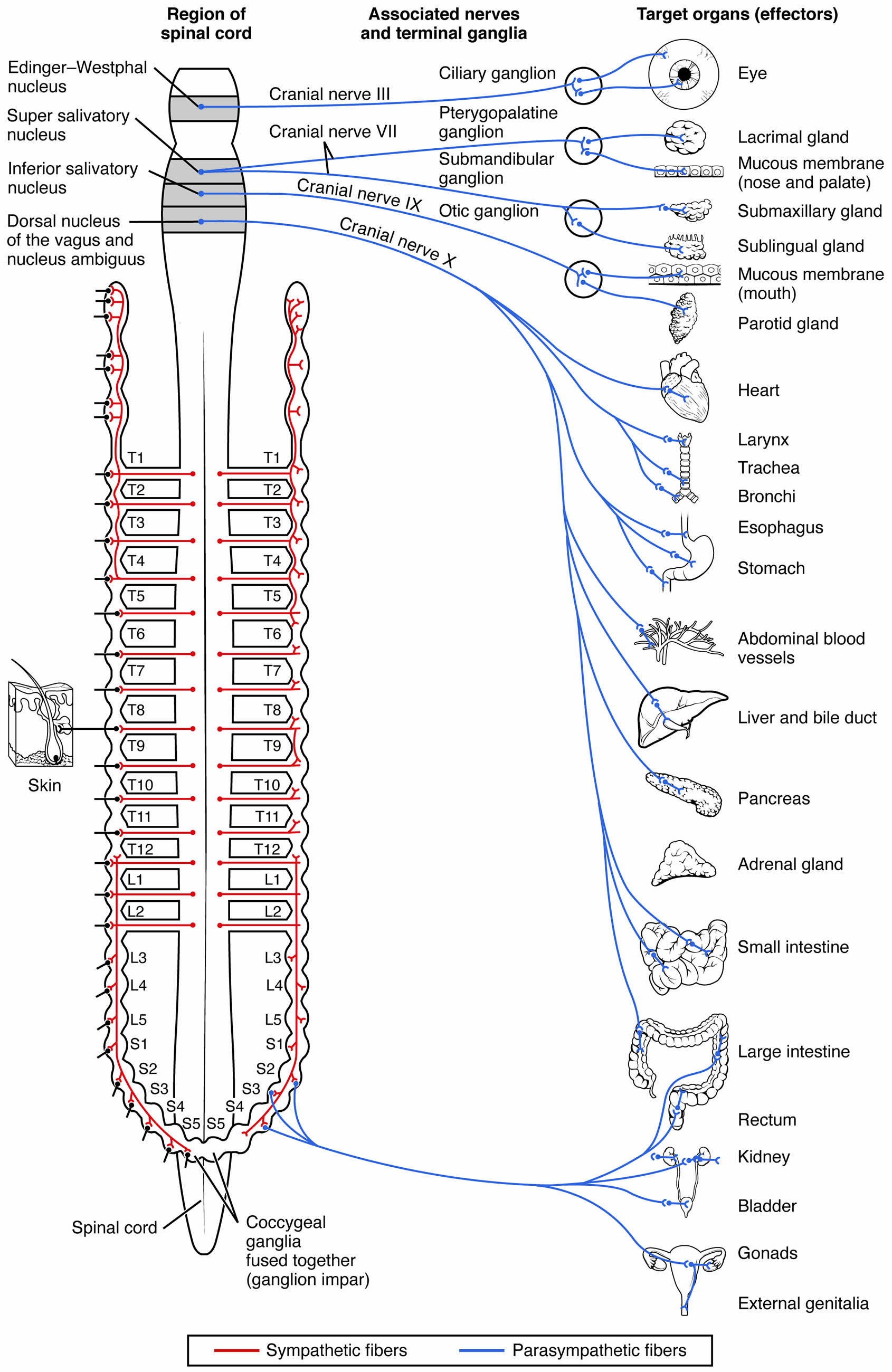
The parasympathetic division of the autonomic nervous system is essential for promoting rest, digestion, and recovery, counterbalancing the sympathetic “fight or flight” response. This diagram illustrates the intricate connections from brainstem nuclei and sacral spinal cord regions to terminal ganglia and target organs, showcasing how this system maintains bodily homeostasis during calm states.
Labels in the Diagram
Edinger-Westphal Nucleus The Edinger-Westphal Nucleus is located in the midbrain and controls pupillary constriction and lens accommodation via cranial nerve III. It plays a key role in focusing the eye during near vision tasks.
Superior Salivatory Nucleus The Superior Salivatory Nucleus, found in the pons, regulates salivary gland secretion through cranial nerve VII. It stimulates saliva production to aid in digestion and oral health.
Inferior Salivatory Nucleus The Inferior Salivatory Nucleus, located in the medulla, governs parotid gland activity via cranial nerve IX. It ensures adequate saliva flow for chewing and swallowing.
Dorsal Nucleus of the Vagus and Nucleus Ambiguus The Dorsal Nucleus of the Vagus and Nucleus Ambiguus, situated in the medulla, control heart rate and gastrointestinal motility via cranial nerve X. These nuclei promote relaxation and digestive efficiency.
Cranial Nerve III The Cranial Nerve III (oculomotor nerve) originates from the Edinger-Westphal nucleus and innervates the ciliary ganglion. It facilitates parasympathetic control of eye muscles for focusing.
Cranial Nerve VII The Cranial Nerve VII (facial nerve) extends from the superior salivatory nucleus to the pterygopalatine and submandibular ganglia. It regulates salivary and lacrimal gland functions.
Cranial Nerve IX The Cranial Nerve IX (glossopharyngeal nerve) connects the inferior salivatory nucleus to the otic ganglion. It supports parotid gland activity for salivary secretion.
Cranial Nerve X The Cranial Nerve X (vagus nerve) arises from the dorsal nucleus of the vagus and nucleus ambiguus, innervating multiple ganglia. It extensively controls thoracic and abdominal organs.
Ciliary Ganglion The Ciliary Ganglion, near the eye, receives input from cranial nerve III and innervates the eye. It adjusts pupil size and lens shape for visual accommodation.
Pterygopalatine Ganglion The Pterygopalatine Ganglion, located near the nasal cavity, is innervated by cranial nerve VII. It stimulates lacrimal and nasal mucous membrane secretions.
Submandibular Ganglion The Submandibular Ganglion, near the submandibular gland, receives cranial nerve VII input. It enhances saliva production for digestive processes.
Otic Ganglion The Otic Ganglion, close to the parotid gland, is supplied by cranial nerve IX. It regulates parotid secretion to support oral moisture.
T1 The T1 segment marks the upper thoracic spinal cord, where sympathetic fibers originate, contrasting with parasympathetic sacral input. It helps delineate the spinal cord’s role in autonomic control.
T2 The T2 segment, another thoracic level, similarly supports sympathetic fibers and provides context for parasympathetic-sacral differences. It highlights the spinal cord’s dual autonomic roles.
T3 The T3 segment continues the thoracic series, emphasizing sympathetic dominance in this region. It contrasts with the parasympathetic focus in sacral areas.
T4 The T4 segment, part of the thoracic spine, reinforces sympathetic activity. It underscores the anatomical separation of autonomic divisions.
T5 The T5 segment, in the mid-thoracic region, further illustrates sympathetic pathways. It provides a reference for understanding parasympathetic distribution.
T6 The T6 segment supports sympathetic innervation in the upper abdomen. It contrasts with the lower sacral parasympathetic input.
T7 The T7 segment continues the sympathetic thoracic series. It highlights the spinal cord’s extensive autonomic network.
T8 The T8 segment, part of the thoracic spine, aids in sympathetic control of upper abdominal organs. It complements the parasympathetic sacral role.
T9 The T9 segment supports sympathetic fibers for abdominal regulation. It contrasts with the parasympathetic influence in pelvic organs.
T10 The T10 segment contributes to sympathetic innervation of the lower abdomen. It provides a transition toward sacral parasympathetic areas.
T11 The T11 segment, near the thoracolumbar junction, supports sympathetic activity. It marks the end of thoracic sympathetic dominance.
T12 The T12 segment, the lowest thoracic level, continues sympathetic control. It serves as a bridge to lumbar and sacral regions.
L1 The L1 segment, in the lumbar spine, marks the start of sympathetic outflow. It contrasts with the parasympathetic sacral input.
L2 The L2 segment, another lumbar level, supports sympathetic fibers. It highlights the thoracolumbar sympathetic origin.
L3 The L3 segment contributes to sympathetic innervation. It provides context for the parasympathetic sacral shift.
L4 The L4 segment, part of the lumbar spine, aids sympathetic control. It contrasts with the sacral parasympathetic focus.
L5 The L5 segment, near the lumbosacral junction, supports sympathetic activity. It transitions toward sacral parasympathetic regions.
S1 The S1 segment, in the sacral spine, initiates parasympathetic outflow. It innervates pelvic organs via terminal ganglia.
S2 The S2 segment, part of the sacral region, continues parasympathetic control. It supports pelvic and genital functions.
S3 The S3 segment enhances parasympathetic innervation of pelvic organs. It plays a role in bladder and reproductive control.
S4 The S4 segment, in the sacral spine, further supports parasympathetic activity. It contributes to pelvic organ regulation.
S5 The S5 segment, the lowest sacral level, completes parasympathetic outflow. It aids in coordinating pelvic functions.
Spinal Cord The Spinal Cord serves as the origin for both sympathetic (thoracolumbar) and parasympathetic (sacral) neurons. It integrates autonomic signals from the brainstem and spinal levels.
Coccygeal Ganglia (Fused Together) The Coccygeal Ganglia (Fused Together), or ganglion impar, is a fused structure at the coccyx. It provides minor parasympathetic input to the pelvic region.
Skin The Skin is primarily influenced by sympathetic fibers for sweating and vasoconstriction. It contrasts with parasympathetic targets like mucous membranes.
Eye The Eye receives parasympathetic innervation via the ciliary ganglion, controlling pupil constriction. This enhances near vision and reduces light exposure.
Lacrimal Gland The Lacrimal Gland produces tears under parasympathetic stimulation from the pterygopalatine ganglion. It maintains eye moisture and health.
Mucous Membrane (Nose and Palate) The Mucous Membrane (Nose and Palate) is moistened by parasympathetic input from the pterygopalatine ganglion. This supports respiratory and olfactory functions.
Submaxillary Gland The Submaxillary Gland secretes saliva via the submandibular ganglion’s parasympathetic control. It aids in digestion and oral lubrication.
Sublingual Gland The Sublingual Gland produces saliva under parasympathetic influence from the submandibular ganglion. It supports digestive enzyme release.
Mucous Membrane (Mouth) The Mucous Membrane (Mouth) is kept moist by parasympathetic innervation from the otic ganglion. This facilitates speech and swallowing.
Parotid Gland The Parotid Gland secretes saliva via the otic ganglion’s parasympathetic input. It contributes to oral health and digestion.
Heart The Heart is slowed by parasympathetic input from the vagus nerve, reducing heart rate. This promotes rest and energy conservation.
Larynx The Larynx is modulated by the vagus nerve to adjust vocal cord tension. This supports relaxed breathing and vocalization.
Trachea The Trachea experiences slight constriction under parasympathetic control from the vagus nerve. This maintains normal airflow during rest.
Bronchi The Bronchi constrict slightly via vagus nerve innervation, reducing air passage. This conserves energy during non-stressful states.
Esophagus The Esophagus enhances motility under vagus nerve control, aiding swallowing. This supports digestive processes during rest.
Stomach The Stomach increases secretion and motility via vagus nerve stimulation. This enhances digestion and nutrient absorption.
Abdominal Blood Vessels The Abdominal Blood Vessels dilate under parasympathetic influence, improving blood flow to digestive organs. This supports metabolic activity.
Liver and Bile Duct The Liver and Bile Duct are modulated by the vagus nerve to regulate bile release. This aids in fat digestion during rest.
Pancreas The Pancreas increases insulin and digestive enzyme secretion via vagus nerve input. This supports glucose metabolism and digestion.
Adrenal Gland The Adrenal Gland is minimally affected by parasympathetic fibers, contrasting with sympathetic stimulation. Its role shifts toward rest-related hormone balance.
Small Intestine The Small Intestine enhances absorption and motility under vagus nerve control. This optimizes nutrient uptake during relaxation.
Large Intestine The Large Intestine increases motility via sacral parasympathetic input, aiding waste elimination. This supports digestive efficiency.
Rectum The Rectum is regulated by sacral parasympathetic fibers to facilitate defecation. This promotes regular bowel function.
Kidney The Kidney experiences slight parasympathetic influence to maintain normal filtration. This contrasts with sympathetic dominance in stress.
Bladder The Bladder contracts and relaxes its sphincter under sacral parasympathetic control. This facilitates urine storage and release.
Gonads The Gonads receive minor parasympathetic input to support reproductive functions. This enhances rest-related hormonal activity.
External Genitalia The External Genitalia are influenced by sacral parasympathetic fibers for sexual response. This promotes reproductive health during relaxation.
Anatomy of the Parasympathetic Nervous System
The parasympathetic division originates from cranial nerves III, VII, IX, and X, as well as sacral spinal segments S2-S4 of the spinal cord. Preganglionic neurons project to terminal ganglia located near or within target organs, where they synapse with short postganglionic fibers.
- Cranial Nuclei: Include the Edinger-Westphal and dorsal vagus nuclei for head and thoracic control.
- Sacral Outflow: Arises from S2-S4 to innervate pelvic organs via coccygeal ganglia.
- Terminal Ganglia: Positioned close to effectors, such as the ciliary and pterygopalatine ganglia.
This proximity allows precise regulation of organ function during restful states.
Physiological Functions of Parasympathetic Activation
The parasympathetic division promotes restorative processes like digestion and energy conservation. Activation of the vagus nerve slows the heart and enhances stomach activity, while sacral fibers support bladder and rectum functions.
- Digestive Stimulation: Increases pancreas enzyme and liver bile secretion.
- Cardiac Regulation: Reduces heart rate for energy savings.
- Excretory Control: Enhances bladder and large intestine motility.
This system ensures the body recovers efficiently after stress.
Clinical Relevance of Parasympathetic Pathways
Understanding the parasympathetic division aids in managing conditions like vagal bradycardia, where excessive vagus nerve activity slows the heart. Knowledge of these pathways supports targeted therapies for autonomic imbalances.
- Vagal Bradycardia: Overactive cranial nerve X leading to low heart rate.
- Neurogenic Bladder: Impaired sacral S2-S4 control affecting urination.
- Therapeutic Options: Vagus nerve stimulation treats epilepsy and depression.
Early diagnosis enhances treatment outcomes for these conditions.
Evolutionary Role and Modern Applications
The parasympathetic division evolved to support rest and reproduction, complementing the sympathetic system’s survival focus. Modern medicine leverages this understanding for innovative treatments.
- Evolutionary Benefit: Enhanced digestion via cranial nerve IX supported early nutrition.
- Medical Advances: Ciliary ganglion manipulation aids glaucoma management.
- Research Directions: Studying sacral outflow improves pelvic health therapies.
Ongoing studies continue to uncover its therapeutic potential.
In conclusion, the parasympathetic division of the autonomic nervous system exemplifies the body’s ability to restore balance through precise neural connections. This diagram provides a clear guide to its pathways, from the spinal cord and cranial nerves to diverse target organs, offering valuable insights for clinical and research applications.

