Discover the fascinating process of hemostasis, where the body works tirelessly to stop bleeding and repair damaged blood vessels. This article delves into the detailed steps of blood clotting, illustrated through a comprehensive diagram, providing an essential guide for understanding this critical physiological mechanism. Explore how the body naturally responds to injury, ensuring minimal blood loss and effective vessel repair.
Labels Introduction
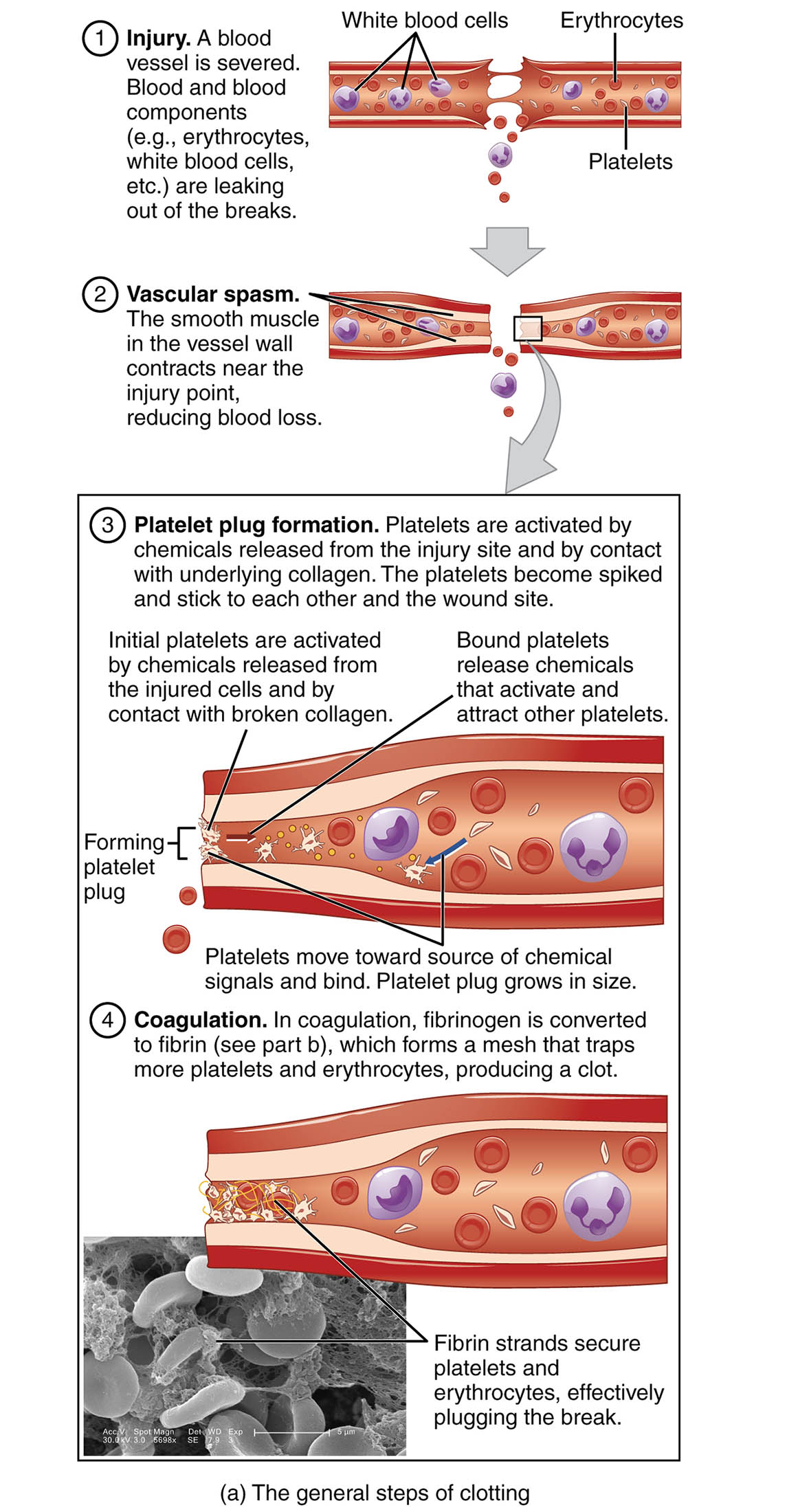
- Injury This initial step occurs when a blood vessel is severed, allowing blood components such as erythrocytes, white blood cells, and platelets to leak out. The disruption triggers the body’s immediate response to prevent excessive blood loss.
- Vascular spasm In this phase, the smooth muscle in the vessel wall contracts near the injury point, reducing blood flow and minimizing further loss. This rapid constriction is a critical first defense mechanism in the hemostasis process.
- Platelet plug formation Here, platelets are activated by chemicals released from the injury site and by contact with underlying collagen, causing them to become spiked and stick together. Bound platelets release additional chemicals that attract and activate other platelets, forming a growing plug to temporarily seal the vessel.
- Coagulation During this stage, fibrinogen is converted to fibrin, which forms a mesh that traps more platelets and erythrocytes, producing a stable clot. Fibrin strands secure the clot, effectively plugging the leak and aiding in vessel wall repair.
Detailed Overview of Hemostasis
Hemostasis is a vital process that prevents excessive bleeding following an injury to a blood vessel. The body employs a series of coordinated steps to achieve this, beginning with the immediate response to vascular damage. This intricate mechanism ensures that blood loss is minimized while the vessel begins to heal.
- The process starts with an injury, where the integrity of the blood vessel is compromised.
- Blood components, including red blood cells (erythrocytes), white blood cells, and platelets, escape through the breach, signaling the need for repair.
- Vascular spasm follows as the vessel constricts, reducing blood flow to the injured area.
- This contraction is mediated by the smooth muscle in the vessel wall, providing an initial barrier against hemorrhage.
- Next, platelet plug formation initiates as platelets respond to the injury.
- Activated by exposed collagen and chemical signals, platelets aggregate to form a temporary seal, a crucial step in halting minor bleeding.
- The final stage, coagulation, involves a complex cascade of reactions.
- Fibrinogen, a soluble plasma protein, is converted into insoluble fibrin strands by the enzyme thrombin, creating a robust mesh.
- This mesh traps additional blood cells, stabilizing the clot and facilitating long-term vessel repair.
The Role of Each Step in Blood Clotting
Understanding each phase of hemostasis reveals its importance in maintaining circulatory health. The initial vascular spasm sets the stage by limiting blood loss almost instantly.
- This rapid response is essential for small vessels, where immediate constriction can prevent significant hemorrhage.
- The effectiveness of this step depends on the severity and location of the injury.
- Platelet plug formation then builds on this foundation, acting as a temporary fix.
- Platelets release adenosine diphosphate (ADP) and thromboxane A2, which enhance aggregation and recruit more platelets to the site.
- This process is particularly vital in capillaries and small arterioles, where a stable plug can suffice.
- Coagulation completes the process by forming a durable clot.
- The conversion of fibrinogen to fibrin involves multiple clotting factors, ensuring a strong and resilient structure.
- This step is critical for larger vessels, where a platelet plug alone may not suffice to stop bleeding.
Physiological Mechanisms Behind Hemostasis
The physiological underpinnings of hemostasis are both fascinating and complex. The injury triggers a cascade that involves both cellular and molecular components.
- Endothelial cells lining the vessel release von Willebrand factor, aiding platelet adhesion.
- This factor bridges platelets to the collagen exposed by the injury.
- During vascular spasm, calcium ions and neurotransmitters play a key role in muscle contraction.
- The duration of the spasm varies, typically lasting minutes to hours depending on the injury’s extent.
- In platelet plug formation, the activation process involves a change in platelet shape and the release of granules.
- These granules contain chemicals that amplify the clotting response, ensuring a robust plug.
- Coagulation relies on the intrinsic and extrinsic pathways converging on the common pathway.
- The end result is a fibrin network that integrates with the platelet plug, providing a scaffold for tissue repair.
Conclusion
The hemostasis process is a remarkable example of the body’s ability to protect itself from injury. From the initial vascular spasm to the final coagulation stage, each step works in harmony to seal wounds and promote healing. This intricate dance of blood components and chemical signals ensures that blood loss is controlled, allowing the vascular system to recover efficiently. By understanding these mechanisms, one gains a deeper appreciation for the body’s natural resilience and the critical role of hemostasis in maintaining health.

