This anatomical comparison diagram illustrates the physiological differences between a healthy vascular system and one compromised by Peripheral Arterial Disease (PAD). The image highlights the progressive narrowing of the arteries in the leg due to the accumulation of plaque, a process known as atherosclerosis, which significantly restricts blood flow and oxygen delivery to the lower extremities.
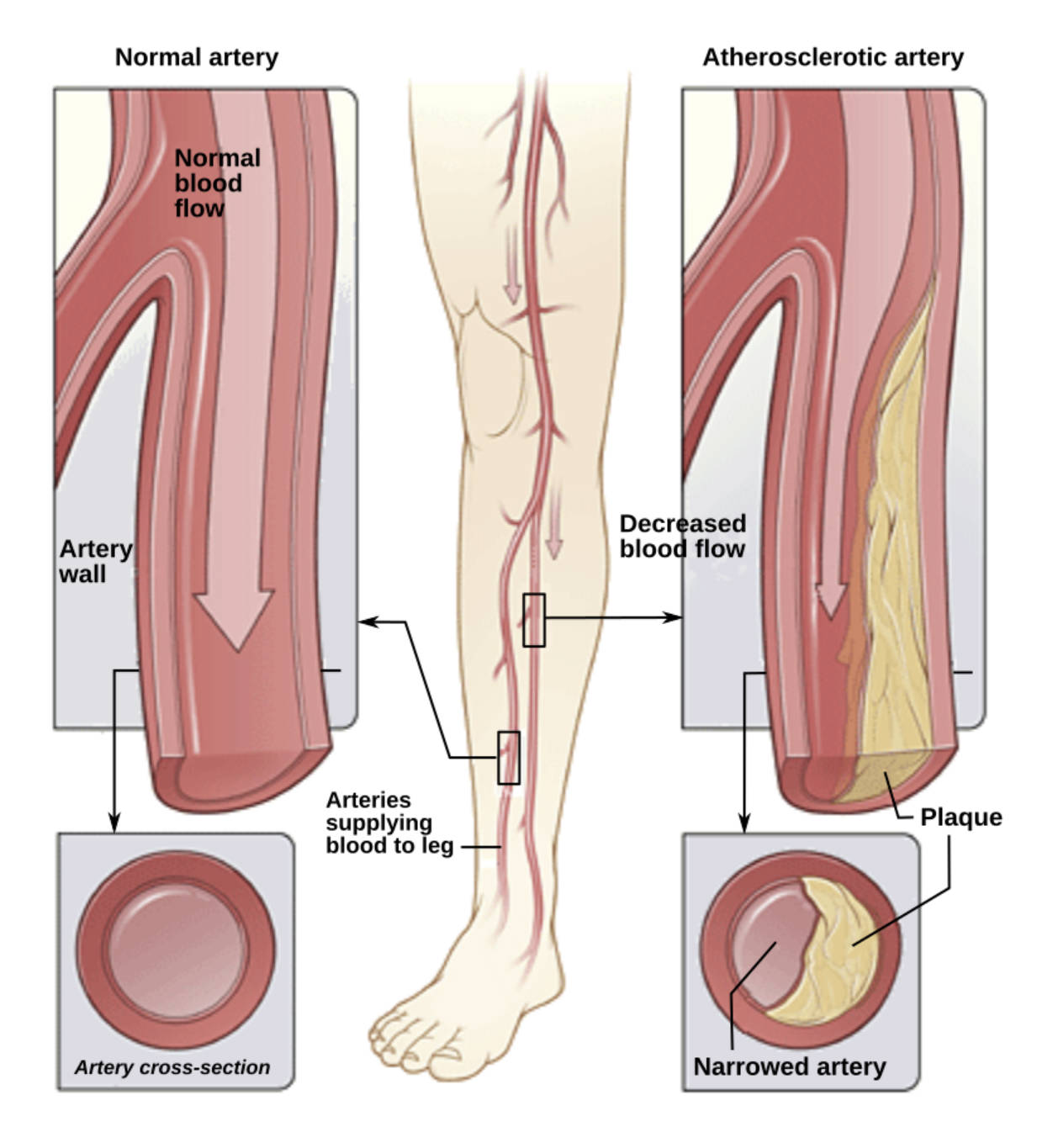
Normal artery: This represents a healthy blood vessel with a smooth, elastic interior lining known as the endothelium. In this state, the artery is flexible and wide enough to handle the volume of blood required by the muscles during both rest and activity.
Normal blood flow: The arrow depicts the unimpeded, laminar movement of oxygen-rich blood traveling from the heart down to the legs and feet. This efficient circulation ensures that tissues receive adequate nutrients and oxygen to function correctly without pain or fatigue.
Artery wall: This label indicates the muscular and elastic layers of the vessel, specifically the tunica media and tunica intima. These walls maintain vascular tone and blood pressure, expanding and contracting rhythmically with the heartbeat.
Artery cross-section: The inset view provides a transverse slice of the vessel, revealing a wide, open lumen (the central space). This circular opening is free of obstruction, allowing for maximum hydraulic efficiency.
Arteries supplying blood to leg: These vessels, typically the femoral, popliteal, and tibial arteries, form the primary vascular highway for the lower limb. The diagram localizes the potential site of blockage within these long vessels that run through the thigh and calf.
Atherosclerotic artery: This vessel exhibits the pathological changes associated with vascular disease, characterized by stiffening and internal damage. The irregular inner surface disrupts blood flow, creating turbulence and reducing the vessel’s ability to dilate in response to exercise.
Decreased blood flow: The thinner arrow visually represents the hemodynamic consequence of the blockage, where the volume and velocity of blood reaching the foot are significantly reduced. This reduction leads to ischemia, a condition where tissue demand for oxygen exceeds the available supply.
Plaque: This yellow substance is a deposit composed of cholesterol, fatty substances, cellular waste products, calcium, and fibrin. Over time, this buildup hardens and intrudes into the arterial lumen, creating a physical barrier to circulation.
Narrowed artery: Also known as stenosis, this label points to the reduced diameter of the vessel caused by the encroaching plaque. The cross-section confirms that the available space for blood to pass through has been drastically minimized.
The Mechanisms of Peripheral Arterial Disease
Peripheral Arterial Disease (PAD) is a common yet serious circulatory problem in which narrowed arteries reduce blood flow to the limbs. As illustrated in the diagram, the disease is primarily caused by atherosclerosis, a systemic hardening of the arteries. While this process can occur in any vessel in the body, when it affects the arteries supplying the legs, it creates a specific set of challenges. The accumulation of lipids and inflammatory cells within the arterial wall begins gradually, often starting years before symptoms appear.
The circulatory system relies on pressure gradients to move blood. In a healthy leg, the arteries are wide smooth tubes that offer little resistance. However, as plaque builds up, the heart must work harder to push blood through the narrowed space. This creates a bottleneck effect. During physical activity, such as walking or climbing stairs, the leg muscles require a significant increase in blood flow to sustain movement. In a patient with PAD, the narrowed arteries cannot accommodate this increased demand, leading to a supply-demand mismatch.
This mismatch manifests clinically as claudication, a cramping pain in the leg induced by exercise and relieved by rest. If the disease progresses unchecked, the reduction in blood flow can become critical, affecting the limb even when the patient is sitting or lying down. Recognizing the anatomical changes shown in the image is the first step toward diagnosis and intervention.
Key risk factors that accelerate the transition from a normal artery to an atherosclerotic one include:
- Smoking, which damages the endothelial lining of the artery.
- Diabetes, which promotes plaque formation and arterial stiffening.
- Hypertension (high blood pressure), which places mechanical stress on arterial walls.
- High cholesterol (hyperlipidemia), which provides the raw material for plaque deposits.
Pathophysiology of Atherosclerosis in the Legs
The transition from a normal artery to a diseased one is a complex biological process. It typically begins with injury to the endothelium, the delicate inner lining of the artery wall. Once this lining is damaged—often by toxins from tobacco smoke or high blood pressure—it becomes permeable to Low-Density Lipoprotein (LDL) cholesterol. These cholesterol particles become trapped within the arterial wall, triggering an immune response. White blood cells called macrophages rush to the site to digest the cholesterol but eventually become overloaded, turning into “foam cells” that form the fatty streak visible in early atherosclerosis.
As the disease advances, smooth muscle cells from the artery wall migrate to cover the fatty deposit, forming a fibrous cap. Underneath this cap, the core of the plaque can become necrotic and calcified, hardening the artery like a pipe clogged with mineral deposits. This condition, atherosclerosis, results in the loss of arterial elasticity. In the lower limbs, this rigidity prevents the vessels from vasodilating (widening) when muscles need more oxygen. If the fibrous cap ruptures, it can cause a sudden blood clot (thrombus) to form, potentially leading to acute limb ischemia, a medical emergency requiring immediate attention to save the leg.
Clinical Consequences and Management
The clinical impact of the narrowed artery shown in the diagram ranges from mild discomfort to severe tissue loss. In early stages, patients may attribute leg pain to aging or arthritis, delaying diagnosis. However, as the lumen narrows further, the condition can progress to Critical Limb Ischemia (CLI). In CLI, the blood flow is so restricted that the skin and tissues of the feet do not receive enough oxygen to survive, leading to non-healing sores, ulcers, or gangrene. This stage often presents with rest pain—a severe burning sensation in the feet that occurs at night when gravity no longer assists blood flow.
Management of PAD focuses on halting the progression of plaque buildup and improving blood flow. Lifestyle modifications, such as smoking cessation and supervised exercise programs, are fundamental. Exercise helps stimulate the growth of collateral vessels—small natural bypasses that form around the blockage. Pharmacological treatments often include antiplatelet agents to prevent clots and statins to lower cholesterol and stabilize the plaque. In severe cases where peripheral arterial disease significantly impairs quality of life or threatens the limb, interventional procedures such as angioplasty (using a balloon to open the artery) or surgical bypass grafting may be necessary to reroute blood flow around the obstruction.
Conclusion
The comparison between a normal and an atherosclerotic artery serves as a vital visual guide to understanding the mechanics of Peripheral Arterial Disease. By visualizing how plaque physically obstructs the vascular pathways in the leg, patients and healthcare providers can better appreciate the importance of maintaining vascular health. Early intervention, aggressive management of risk factors, and monitoring for symptoms of claudication are essential strategies to prevent the progression from a narrowed artery to critical ischemia.

