Explore the anatomical features of a heart affected by a Patent Ductus Arteriosus (PDA), a common congenital heart defect, as illustrated in this cross-section diagram. This detailed explanation will illuminate the implications of this condition on normal blood flow and its potential health consequences. Understanding PDA is crucial for early diagnosis and effective management in newborns and infants.
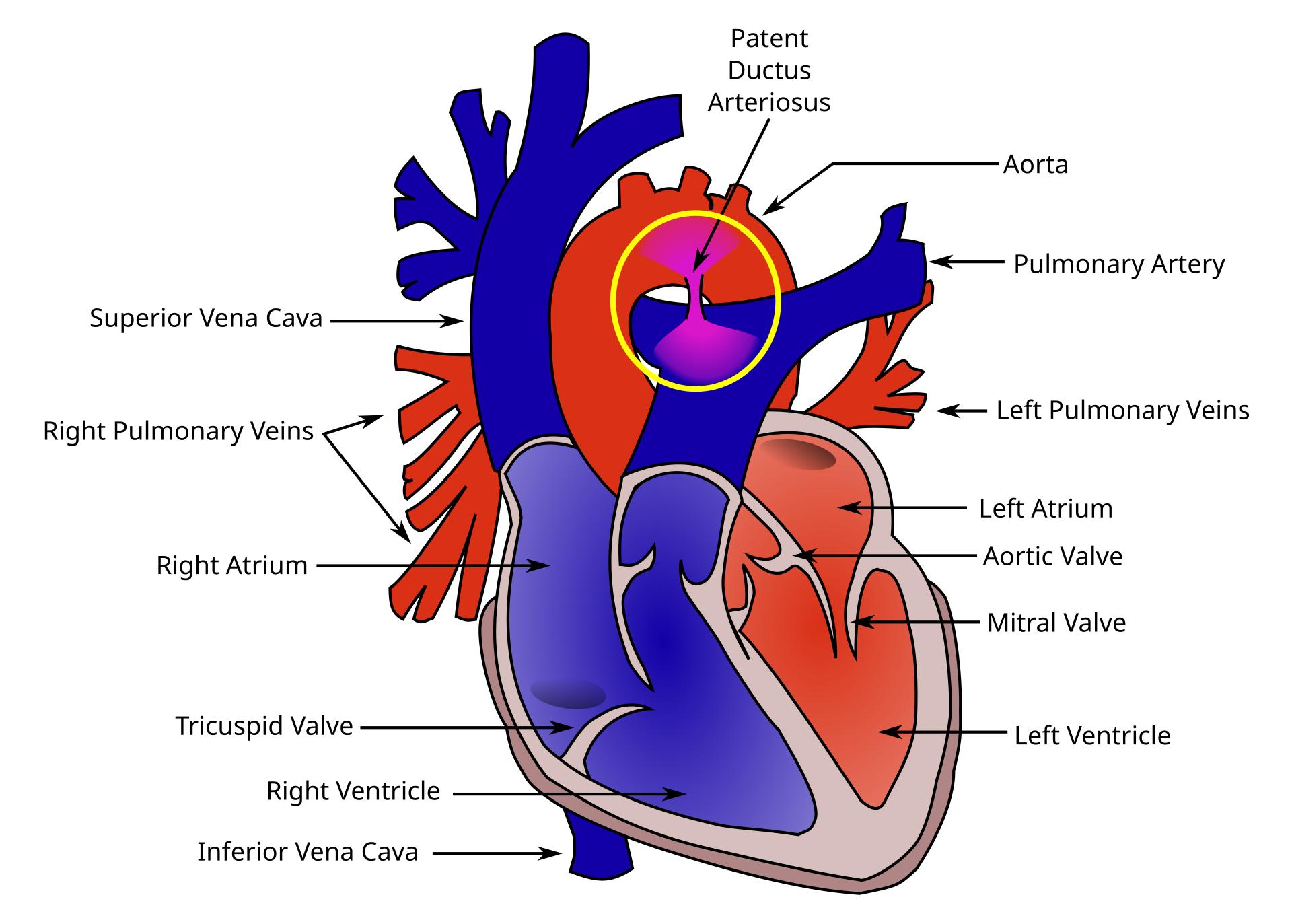
This image provides a cross-sectional view of the heart, prominently featuring a Patent Ductus Arteriosus (PDA) alongside other key cardiac structures. The labels help to understand both normal anatomy and the defect.
Patent Ductus Arteriosus: This label points to an open connection (shunt) between the aorta and the pulmonary artery, which normally closes shortly after birth. In cases of PDA, this fetal blood vessel remains open, leading to abnormal blood flow.
Aorta: The largest artery in the body, originating from the left ventricle, responsible for distributing oxygenated blood to the entire systemic circulation. In PDA, blood can abnormally shunt from the aorta into the pulmonary artery.
Pulmonary Artery: This major artery carries deoxygenated blood from the right ventricle to the lungs for oxygenation. In PDA, it receives an abnormal flow of oxygenated blood from the aorta, leading to increased pulmonary blood flow.
Superior Vena Cava: A large vein that collects deoxygenated blood from the upper half of the body and delivers it to the right atrium. It represents a key component of the systemic venous return.
Right Pulmonary Veins: These veins return oxygenated blood from the right lung to the left atrium. They are essential for completing the pulmonary circuit and delivering oxygen-rich blood to the heart.
Right Atrium: The upper-right chamber of the heart that receives deoxygenated blood from the body via the superior and inferior vena cava. It acts as a collecting chamber before pumping blood into the right ventricle.
Tricuspid Valve: Located between the right atrium and the right ventricle, this valve prevents the backflow of deoxygenated blood into the right atrium when the right ventricle contracts. Its proper function is critical for unidirectional flow on the right side of the heart.
Right Ventricle: The lower-right chamber of the heart, responsible for pumping deoxygenated blood to the lungs through the pulmonary artery. In PDA, the right ventricle may face increased workload due to the increased pulmonary blood flow.
Inferior Vena Cava: A large vein that collects deoxygenated blood from the lower half of the body and delivers it to the right atrium. It is another primary vessel for systemic venous return.
Left Pulmonary Veins: These veins return oxygenated blood from the left lung to the left atrium. Along with the right pulmonary veins, they complete the pulmonary circuit, bringing oxygen-rich blood to the heart.
Left Atrium: The upper-left chamber of the heart that receives oxygenated blood from the lungs via the pulmonary veins. It then pumps this blood into the left ventricle.
Aortic Valve: This valve is situated between the left ventricle and the aorta, regulating the flow of oxygenated blood out of the heart into systemic circulation. Its proper functioning is critical for maintaining systemic blood pressure.
Mitral Valve: Also known as the bicuspid valve, this valve is located between the left atrium and the left ventricle. It ensures that oxygenated blood flows in one direction from the atrium to the ventricle, preventing backflow during ventricular contraction.
Left Ventricle: The lower-left chamber of the heart and the most muscular chamber, responsible for pumping oxygenated blood into the aorta and to the rest of the body. Its powerful contractions generate the high pressure needed for systemic circulation.
Patent Ductus Arteriosus (PDA) is a congenital heart defect that occurs when a fetal blood vessel, the ductus arteriosus, fails to close shortly after birth. During fetal development, the ductus arteriosus is a normal connection between the pulmonary artery and the aorta, allowing blood to bypass the non-functional lungs. However, after birth, as the lungs begin to function and systemic blood pressure increases, this shunt is supposed to close. When it remains open, it results in an abnormal communication between the two major arteries, leading to a left-to-right shunt.
The consequence of a Patent Ductus Arteriosus is that oxygenated blood, which has just been pumped by the left ventricle into the high-pressure aorta, shunts back into the lower-pressure pulmonary artery. This means that blood that should be going to the body is recirculated through the lungs, increasing blood flow to the pulmonary circulation. This can lead to several problems, depending on the size of the PDA and the amount of shunting. In infants, a large PDA can cause symptoms such as rapid breathing, poor feeding, poor weight gain, and increased susceptibility to respiratory infections.
Over time, a significant PDA can lead to complications such as pulmonary hypertension, where the increased blood flow to the lungs causes the blood vessels in the lungs to narrow and thicken. This, in turn, can put a strain on the right side of the heart, potentially leading to right-sided heart failure. In severe, untreated cases, it can even lead to Eisenmenger syndrome, a condition where the shunt reverses direction, sending deoxygenated blood to the body. Early diagnosis, often through echocardiography, and treatment, which can range from medications to surgical closure, are crucial to prevent these long-term complications.
- PDA is more common in premature infants.
- A characteristic “machine-like” murmur can often be heard on auscultation.
- Prostaglandin inhibitors, such as indomethacin, can sometimes be used to medically close a PDA in premature infants.
- Surgical ligation or catheter-based device closure are common treatment options for persistent PDA.
This detailed illustration provides valuable insight into the anatomical presentation of Patent Ductus Arteriosus, clearly demonstrating the abnormal connection between the aorta and pulmonary artery. Understanding this congenital heart defect is critical for medical professionals in pediatrics and cardiology for prompt diagnosis and intervention. Early management of PDA is essential to prevent adverse effects on the heart and lungs, ensuring healthier outcomes for affected individuals.

