This diagram illustrates the intricate process of Coronary Artery Bypass Graft (CABG) surgery, a vital procedure designed to restore healthy blood flow to the heart muscle. When coronary arteries become blocked or severely narrowed due to plaque buildup, CABG provides an alternate route for blood, alleviating symptoms and improving cardiac function. It showcases the types of grafts used and their strategic placement to bypass diseased segments.
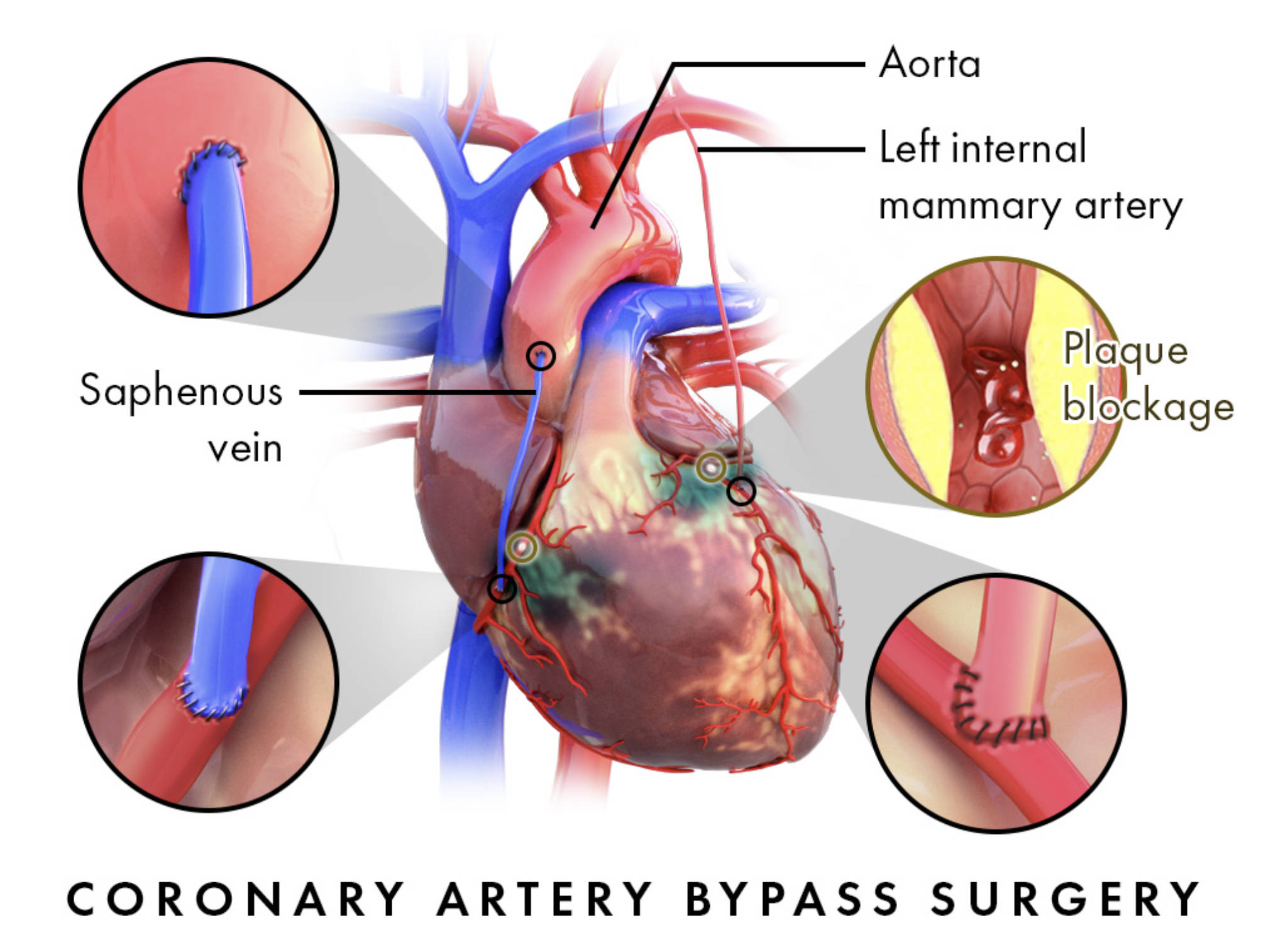
Labels Explanation:
Aorta: The largest artery in the body, originating from the left ventricle of the heart and extending down to the abdomen. It distributes oxygenated blood to all parts of the body, and in CABG, it often serves as the primary connection point for bypass grafts.
Left internal mammary artery: Also known as the left internal thoracic artery, this blood vessel is located inside the chest wall. It is frequently used as a graft in CABG due to its excellent long-term patency rates and its proximity to the heart, making it a highly preferred choice for bypass.
Saphenous vein: A large, superficial vein located in the leg, commonly harvested for use as a bypass graft. Segments of this vein are removed and then surgically connected to bypass blocked coronary arteries, creating new pathways for blood flow to the heart muscle.
Plaque blockage: This refers to the accumulation of fatty deposits, cholesterol, cellular waste products, calcium, and fibrin within the inner lining of an artery. This buildup, known as atherosclerosis, narrows the artery, restricts blood flow, and is the primary reason for performing CABG surgery.
Introduction to Coronary Artery Bypass Graft (CABG) Surgery
Coronary Artery Bypass Graft (CABG) surgery is a critical surgical intervention for individuals suffering from severe coronary artery disease (CAD). This condition arises when the arteries supplying blood to the heart muscle become hardened and narrowed due to the buildup of plaque, a process known as atherosclerosis. When these blockages significantly impede blood flow, the heart muscle can be deprived of essential oxygen and nutrients, leading to symptoms such as chest pain (angina), shortness of breath, and in severe cases, a heart attack. The primary objective of CABG is to circumvent these blockages by creating new pathways for blood, thereby improving perfusion to the heart muscle.
The procedure involves harvesting healthy blood vessels, known as grafts, from other parts of the patient’s body. These grafts are then surgically connected to the coronary arteries, effectively bypassing the narrowed or blocked segments. The choice of graft material is crucial for the long-term success of the surgery. Common sources for these grafts include:
- Left internal mammary artery (LIMA): Often considered the gold standard due to its excellent long-term patency.
- Saphenous vein: Harvested from the leg, these grafts are widely used, especially for multiple bypasses.
- Radial artery: Taken from the arm, it offers another arterial graft option.
CABG is typically recommended for patients with multiple vessel disease, significant blockages not amenable to less invasive treatments like angioplasty and stenting, or those with impaired left ventricular function. The decision to proceed with CABG is made after a thorough evaluation by a multidisciplinary heart team, considering the patient’s overall health, the extent of their CAD, and potential risks versus benefits.
Understanding Coronary Artery Disease (CAD)
Coronary artery disease (CAD) is the most common type of heart disease and a leading cause of death worldwide. It occurs when the coronary arteries—the blood vessels that supply blood to the heart muscle—become damaged and narrowed. The primary cause of CAD is atherosclerosis, a gradual process where plaque accumulates on the inner walls of the arteries. This plaque, composed of cholesterol, fats, calcium, and other substances, hardens and narrows the arterial lumen, reducing blood flow. Over time, this reduction in blood flow can cause various symptoms and complications.
When the heart muscle doesn’t receive enough oxygenated blood, it can lead to angina, which is chest pain or discomfort. If a plaque ruptures, it can trigger the formation of a blood clot that completely blocks the artery, resulting in a heart attack. Long-term, chronic deprivation of blood flow can weaken the heart muscle, leading to heart failure. Risk factors for CAD include high blood pressure, high cholesterol, diabetes, smoking, obesity, lack of physical activity, and a family history of heart disease. Lifestyle modifications, medications, and sometimes surgical interventions like CABG are essential for managing CAD and preventing its progression.
The CABG Procedure and Post-Operative Care
The CABG procedure is a major surgery typically performed under general anesthesia and can last several hours. During the operation, a surgeon usually makes an incision down the center of the chest to access the heart. In many cases, the heart is temporarily stopped, and a heart-lung machine takes over the functions of the heart and lungs, a technique known as “on-pump” CABG. This allows the surgeon to operate on a still heart. However, “off-pump” or “beating-heart” CABG is also an option for some patients, where the surgery is performed while the heart continues to beat. The surgeon then meticulously grafts the chosen vessels to bypass the blocked coronary arteries. One end of the graft is typically attached to the aorta, and the other end to the coronary artery beyond the blockage, effectively restoring blood flow.
Following CABG surgery, patients are closely monitored in an intensive care unit (ICU) for a few days before being transferred to a regular hospital ward. Recovery is a gradual process that requires patience and adherence to medical advice. Post-operative care involves pain management, wound care, and a progressive increase in physical activity. Cardiac rehabilitation is a crucial component of recovery, offering supervised exercise programs, education on heart-healthy living, and counseling to help patients regain strength and reduce future cardiovascular risks. Full recovery can take several weeks to months, but the long-term benefits of improved blood flow to the heart can significantly enhance a patient’s quality of life and longevity. Adopting a heart-healthy lifestyle, including a balanced diet, regular exercise, and medication adherence, is vital for the continued success of the bypass grafts.
CABG surgery stands as a powerful testament to modern medicine’s ability to address severe coronary artery disease, offering a second chance at a healthier life for countless individuals. By meticulously rerouting blood flow around life-threatening blockages, this procedure not only alleviates debilitating symptoms but also significantly improves long-term cardiac outcomes. The journey through CABG and recovery underscores the importance of both advanced surgical skill and the patient’s commitment to ongoing heart health management.

