This computed tomography (CT) image provides a detailed view of atherosclerosis affecting the abdominal aorta in a 70-year-old woman with a history of hypertension and dyslipidemia. We will explore the key features highlighted in this scan, discuss the underlying medical condition, and provide comprehensive insights into its implications for patient health. This analysis aims to enhance understanding of a common cardiovascular concern in an aging population.
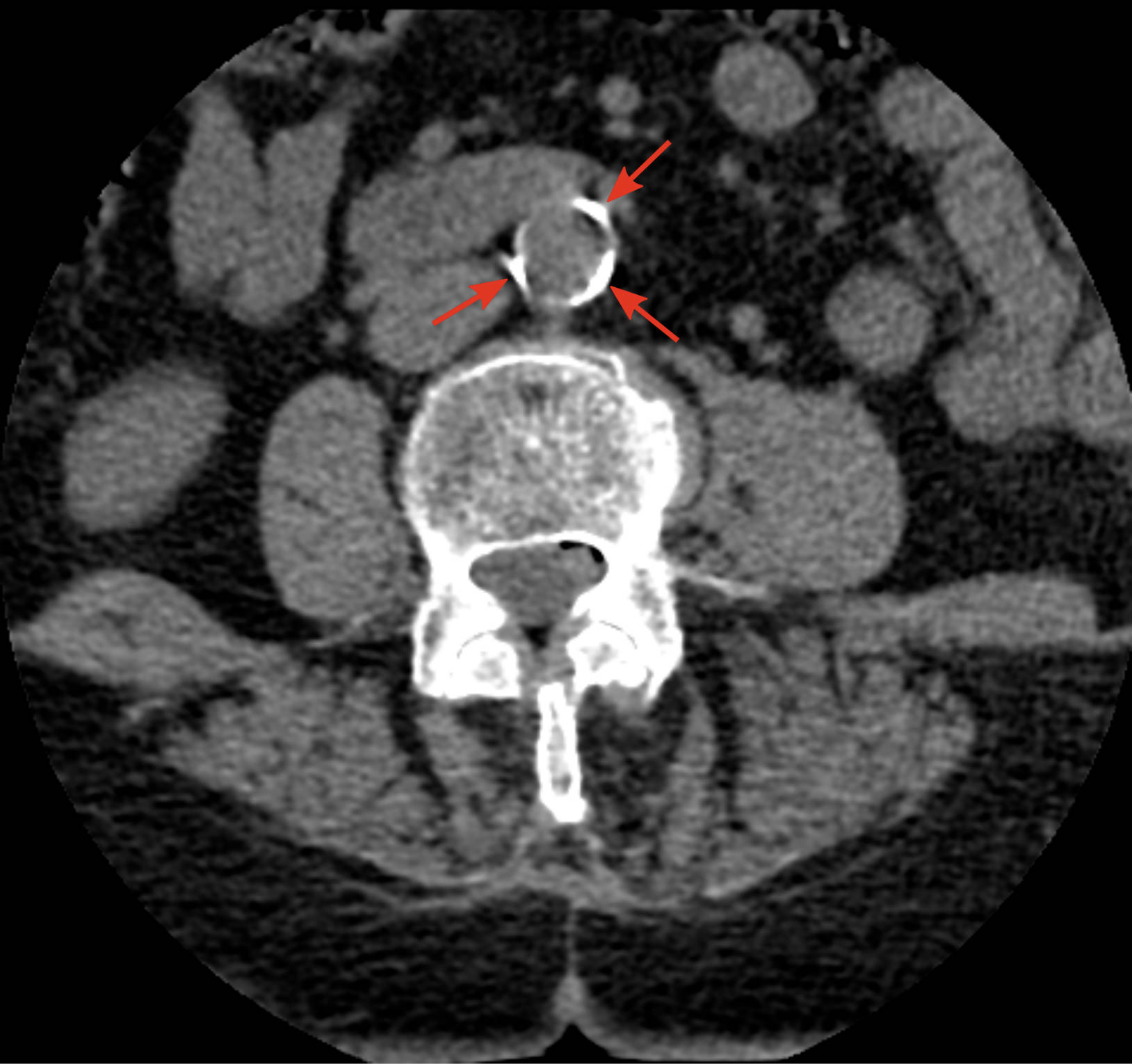
Arrows: These arrows point to significant calcifications within the wall of the abdominal aorta, indicative of advanced atherosclerosis. These calcified plaques narrow the arterial lumen and reduce the elasticity of the vessel, impeding normal blood flow. Such findings are critical in assessing cardiovascular risk and guiding treatment strategies.
Introduction to Abdominal Aortic Atherosclerosis
Atherosclerosis is a chronic inflammatory disease characterized by the buildup of plaque within the arterial walls, leading to hardening and narrowing of the arteries. When this process affects the abdominal aorta, the largest artery in the abdomen, it can have serious health consequences. This condition is particularly prevalent in older adults, often exacerbated by coexisting conditions such as hypertension and dyslipidemia, as seen in our patient. Understanding the progression and impact of abdominal aortic atherosclerosis is crucial for effective patient management and preventive care.
The presence of calcified plaques, as visible in the CT scan, signifies a long-standing atherosclerotic process. These calcifications are not merely inert deposits but rather markers of ongoing vascular damage. The stiffening of the aorta due to these plaques increases the workload on the heart and can lead to various complications.
Patients with abdominal aortic atherosclerosis often exhibit several risk factors that contribute to the development and progression of the disease. These factors collectively create an environment conducive to plaque formation and arterial damage. Key risk factors include:
- Hypertension: High blood pressure places increased stress on arterial walls, promoting endothelial damage and plaque formation.
- Dyslipidemia: Elevated levels of low-density lipoprotein (LDL) cholesterol and triglycerides contribute to the deposition of fatty streaks that evolve into atherosclerotic plaques.
- Diabetes Mellitus: High blood sugar levels can damage blood vessels and accelerate atherosclerosis.
- Smoking: Chemical toxins in cigarette smoke directly injure the endothelium and promote inflammation.
- Obesity: Excess body weight is associated with a higher incidence of hypertension, dyslipidemia, and insulin resistance, all risk factors for atherosclerosis.
Recognizing and managing these risk factors is paramount in mitigating the progression of abdominal aortic atherosclerosis and preventing its complications. Early intervention and lifestyle modifications can significantly improve patient outcomes.
The Pathophysiology of Atherosclerosis
Atherosclerosis begins with damage to the endothelium, the inner lining of the artery. This damage can be caused by various factors, including high blood pressure, elevated cholesterol levels, smoking, and diabetes. Once the endothelium is compromised, LDL cholesterol particles can penetrate the arterial wall and become oxidized. Macrophages, a type of white blood cell, then engulf these oxidized LDL particles, transforming into foam cells. These foam cells accumulate, forming fatty streaks that are the earliest visible lesions of atherosclerosis.
Over time, these fatty streaks progress into fibrous plaques. Smooth muscle cells migrate from the media (middle layer) of the artery to the intima (inner layer) and proliferate, laying down collagen and forming a fibrous cap over the lipid core. Calcium also begins to deposit within these plaques, leading to the calcifications observed in the provided CT image. These calcified plaques harden the arterial walls, reducing their elasticity and narrowing the lumen. The compromised blood flow can lead to a range of symptoms, from mild discomfort to severe, life-threatening events. The aorta, being a major conduit for blood distribution, is particularly vulnerable to the systemic effects of this disease.
Clinical Implications and Management
The clinical implications of abdominal aortic atherosclerosis are diverse and depend on the extent and location of the plaque buildup. Narrowing of the abdominal aorta can reduce blood flow to the kidneys, intestines, and lower extremities. This can manifest as renal artery stenosis, mesenteric ischemia, or peripheral artery disease, respectively. Furthermore, the weakened and calcified arterial wall is at an increased risk of developing an aortic aneurysm, a balloon-like bulge that can rupture, leading to catastrophic internal bleeding.
Management strategies for abdominal aortic atherosclerosis focus on reducing risk factors, preventing plaque progression, and treating complications. Lifestyle modifications, such as adopting a heart-healthy diet, regular physical activity, and smoking cessation, are fundamental. Pharmacological interventions often include medications to lower blood pressure (antihypertensives), reduce cholesterol levels (statins), and prevent blood clot formation (antiplatelet agents). In cases of severe stenosis or aneurysm formation, surgical interventions like angioplasty, stenting, or open repair may be necessary to restore blood flow or prevent rupture. Regular monitoring with imaging studies like CT scans helps track disease progression and guide treatment decisions.
Concluding Thoughts on Aortic Health
Understanding the intricacies of abdominal aortic atherosclerosis, especially in individuals with established risk factors like hypertension and dyslipidemia, is paramount for both clinicians and patients. The CT image serves as a powerful diagnostic tool, visually confirming the presence and extent of calcified plaques. By integrating detailed imaging findings with comprehensive patient history, healthcare providers can formulate tailored management plans aimed at mitigating disease progression, preventing severe complications, and ultimately enhancing the patient’s quality of life. Proactive screening and diligent management of cardiovascular risk factors remain the cornerstone of addressing this prevalent condition.

