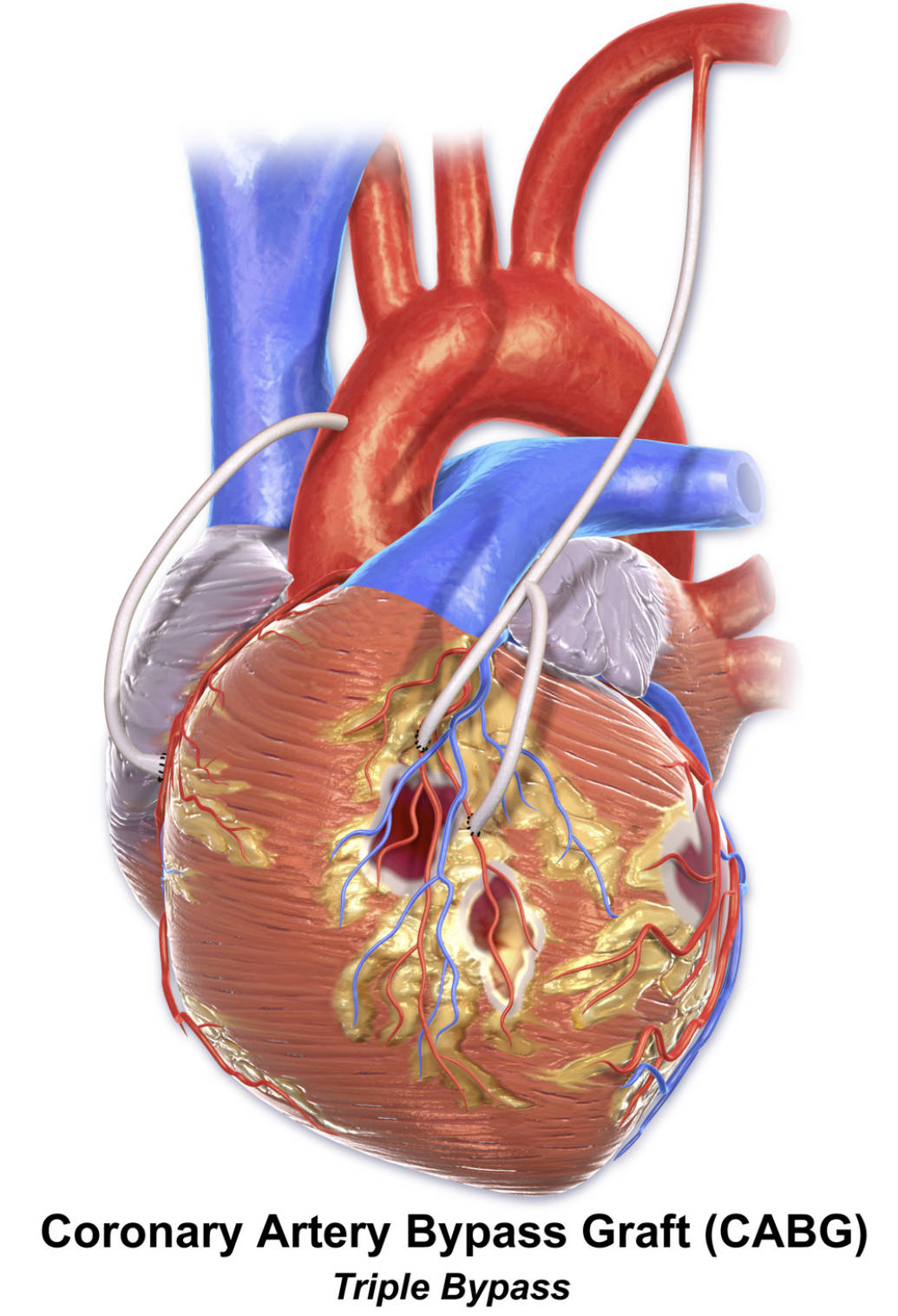
This diagram offers a detailed visual explanation of a triple Coronary Artery Bypass Graft (CABG) procedure, clearly illustrating how three distinct grafts are strategically utilized to bypass significant blockages in three different coronary arteries. This extensive surgical intervention is critical for patients diagnosed with widespread multi-vessel coronary artery disease, where multiple major vessels supplying the heart muscle are severely compromised. Understanding the complexities and precision of a triple bypass, as depicted, is essential for appreciating its role in comprehensively restoring blood flow and significantly improving cardiac function in advanced cases of coronary artery disease.
Introduction to Triple Bypass CABG
Coronary Artery Bypass Graft (CABG) surgery is a cornerstone in the treatment of advanced coronary artery disease (CAD), a condition characterized by the accumulation of atherosclerotic plaque that narrows or blocks the heart’s vital arteries. When three or more of these major arteries are severely obstructed, leading to significant impairment of blood flow to the myocardium, a “triple bypass” CABG is often the recommended course of action. This complex surgical procedure, vividly illustrated in the accompanying diagram, involves creating three new pathways to circumvent critical blockages in three separate coronary arteries. This comprehensive revascularization strategy is designed for patients with extensive multi-vessel CAD.
The primary objective of a triple bypass is to restore robust blood flow to three distinct regions of the heart muscle that are suffering from insufficient oxygen supply due to widespread and severe blockages. This intricate surgery typically involves harvesting healthy blood vessels from the patient’s own body—such as the internal mammary artery from the chest and/or segments of the saphenous vein from the leg—to serve as bypass grafts. These grafts are then meticulously connected to the coronary arteries, effectively creating detours around the diseased segments. The result is a substantial improvement in oxygenation of the affected heart muscle, leading to profound symptom relief, enhanced cardiac function, and a significantly improved quality of life.
The decision to perform a triple bypass is made after a thorough diagnostic evaluation, most notably coronary angiography, which provides a detailed map of the location and severity of all arterial blockages. This highly individualized surgical strategy is crucial for optimizing outcomes in patients with diffuse and severe coronary artery disease that cannot be adequately addressed by less extensive bypasses or less invasive interventions.
Key indications that often lead to a triple bypass CABG include:
- Significant blockages in three major coronary arteries: When three distinct arteries have critical stenoses requiring surgical intervention.
- Widespread ischemic symptoms: Persistent angina, shortness of breath, or other signs of heart muscle ischemia not controlled by medical therapy.
- Extensive multi-vessel disease: Particularly when blockages are complex or involve critical branches.
- Left Main Coronary Artery (LMCA) disease with additional two-vessel involvement: A common scenario necessitating triple bypass.
- Diabetes mellitus with multi-vessel CAD: Patients with diabetes and widespread CAD often benefit significantly from CABG.
- Failed or unsuitable percutaneous coronary intervention (PCI): When stents cannot effectively open or sustain patency in multiple complex lesions.
These factors are meticulously evaluated by the cardiac surgical team to formulate the most effective and durable revascularization plan.
Understanding the Progression of Multi-Vessel CAD
The heart’s consistent demand for oxygen and nutrients is met by the coronary arteries, including the left anterior descending (LAD) artery, the circumflex artery (LCx), and the right coronary artery (RCA), along with their numerous branches. These vessels are highly susceptible to atherosclerosis, a progressive disease characterized by the buildup of fatty plaques, cholesterol, and other substances within their walls. When this process becomes extensive, it can lead to severe narrowings or complete blockages in three or more of these major arteries, a condition referred to as triple-vessel disease.
In such cases, large areas of the heart muscle are deprived of adequate oxygen (ischemia), leading to widespread symptoms and a significantly increased risk of major adverse cardiovascular events. The heart has to work much harder to pump blood through these obstructed pathways, which can eventually lead to weakening of the heart muscle and the development of heart failure. A triple bypass is specifically designed to address these multiple, critical obstructions, ensuring that all three compromised regions of the heart receive a renewed and sufficient blood supply. By comprehensively restoring flow to multiple vessels, the overall function of the heart can be substantially improved, and the long-term progression of the disease mitigated.
The Triple Bypass Procedure: Grafting Multiple Arteries
A triple bypass CABG is a complex open-heart procedure that requires exceptional surgical skill to create three new conduits for blood flow around three separate blockages in the coronary arteries. The surgery is performed under general anesthesia, and the patient is typically placed on a heart-lung machine (cardiopulmonary bypass) to temporarily support circulation while the heart is stopped, allowing the surgeon to work on a motionless field.
Commonly used graft vessels for a triple bypass include a combination of arterial and venous conduits:
- Internal Mammary Artery (IMA): The left internal mammary artery (LIMA) is almost invariably used for a triple bypass, often directed to bypass a blockage in the left anterior descending (LAD) artery due to its superior long-term patency.
- Saphenous Vein Grafts (SVG): Segments of the saphenous vein, typically harvested from the leg, are commonly used for the remaining two grafts. These vein segments are prepared, reversed, and then connected from the aorta to the other two blocked coronary arteries (e.g., the right coronary artery and a major branch of the circumflex artery) distal to their obstructions.
- Radial Artery: In some cases, the radial artery from the arm may be used as an additional arterial graft, particularly when multiple arterial grafts are desired for improved longevity.
The surgical team meticulously selects the appropriate grafts and precisely performs the anastomoses (connections) to ensure the creation of robust and durable new blood flow pathways around all three diseased segments. The diagram vividly illustrates these three distinct grafts providing blood flow to different areas of the heart.
Recovery and Long-Term Outlook After Triple Bypass
Recovery from a triple bypass CABG is a demanding yet ultimately rewarding process. Patients will spend time in an intensive care unit immediately following surgery for close monitoring, followed by a transition to a standard hospital ward. Comprehensive pain management, diligent wound care for both the chest incision and graft harvest sites, and gradual physical mobilization are paramount during the early recovery phase. Participation in a structured cardiac rehabilitation program is crucial and highly beneficial. These programs offer supervised exercise, dietary counseling, stress management techniques, and extensive education on managing cardiovascular risk factors, all tailored to facilitate optimal recovery and improve long-term health.
The long-term outlook for patients who undergo a triple bypass CABG is generally excellent, with substantial improvements in symptoms, quality of life, and often, an extension of life expectancy. Patients frequently experience profound relief from angina and an enhanced ability to engage in daily activities. However, it is critical to understand that while CABG addresses the anatomical blockages, it does not cure the underlying atherosclerosis. Therefore, a lifelong commitment to a heart-healthy lifestyle is absolutely essential. This includes adhering to a balanced diet, maintaining regular physical activity, abstaining from smoking, and meticulously managing conditions such as high blood pressure, high cholesterol, and diabetes. Regular follow-up with a cardiologist is crucial to monitor the patency of all grafts and the overall cardiac health, ensuring the sustained benefits of this life-saving procedure.

