Breaking the Blueprint: The Seventh Person Cured of HIV Challenges Long-Held Medical Beliefs
A 60-year-old German man has officially become the seventh person in the world to be declared “cured” of HIV. His case, detailed in a study published in the journal Nature on December 1, 2025, marks a significant turning point in virology. Perhaps most importantly, he is only the second person to achieve this feat using stem cells that were not inherently resistant to HIV.
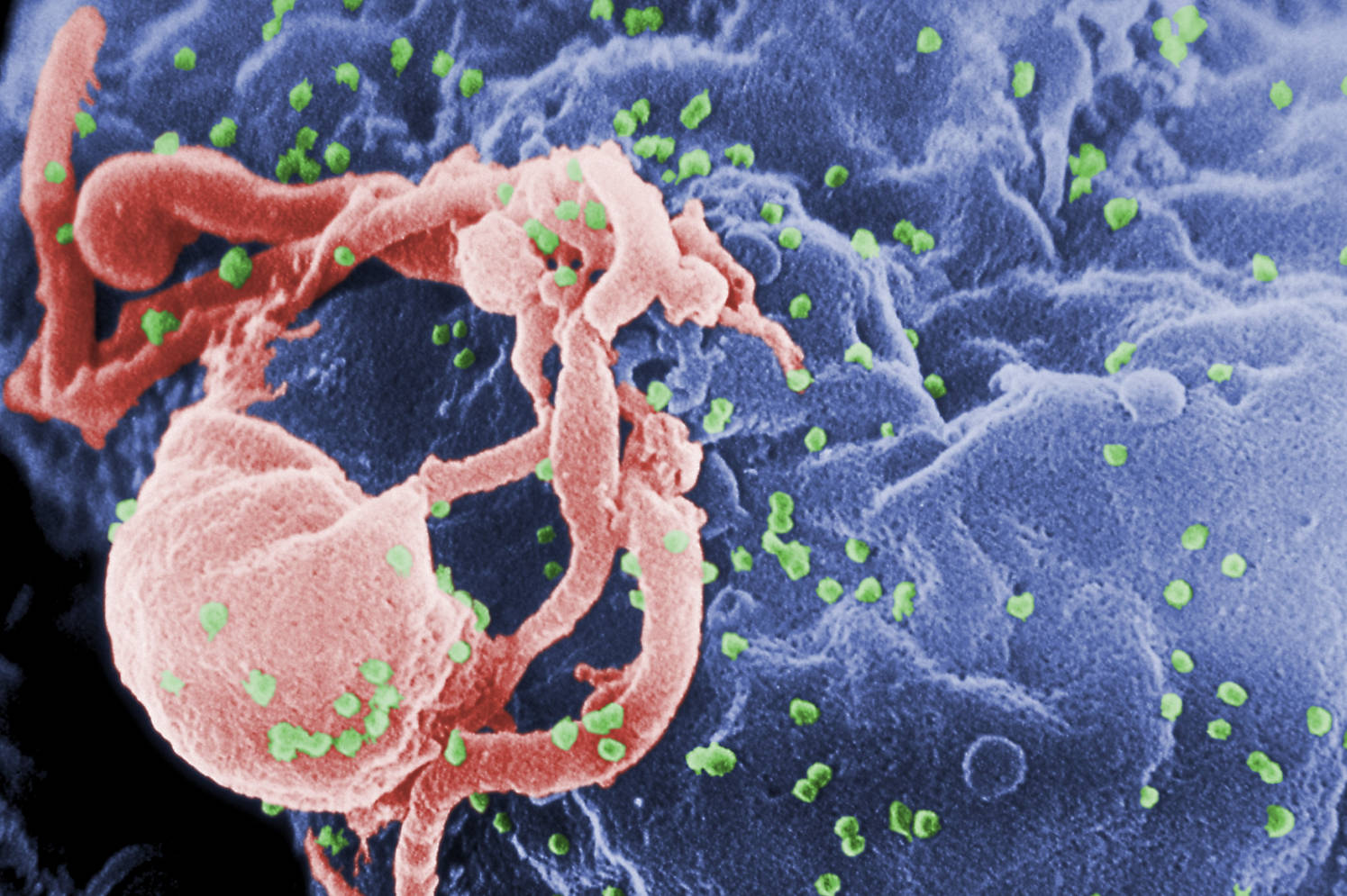
For years, the scientific community believed that “curing” HIV required a very specific biological “key”: a donor with two copies of the CCR5-delta32 genetic mutation. This mutation effectively locks the door that HIV uses to enter immune cells. However, this new case—and a similar one in Geneva—proves that the path to a cure may be broader than we once imagined.
The Case of the “Next Berlin Patient”
The patient, who chooses to remain anonymous, was diagnosed with HIV in 2009 and later developed acute myeloid leukemia (AML), a life-threatening blood cancer. In October 2015, he underwent a stem cell transplant to treat the leukemia.
Because no donor with the rare “double-mutation” (homozygous CCR5-Δ32) was available, doctors used a donor who carried only one copy of the mutation (heterozygous).
Key milestones of his journey include:
- 2015: Received a stem cell transplant for leukemia while continuing Anti-Retroviral Therapy (ART).
- 2018: After three years of stable health and cancer remission, the patient chose to stop taking HIV medication (ART).
- 2024: He has now remained virus-free for 7 years and 3 months without any medication.
Why This Discovery Matters
According to Christian Gaebler, a lead author of the study from Charité – Universitätsmedizin Berlin, this case shifts our understanding of how the virus can be eradicated. “The fact that he was cured without the traditional ‘resistant’ stem cells provides us with many more options for future treatments,” Gaebler noted.
What allowed the cure to happen?
Scientists believe several factors worked together:
- The “Graft-versus-HIV” Effect: The donor’s new immune cells likely recognized the patient’s original, HIV-infected cells as foreign and destroyed them.
- Speed of Replacement: The donor cells replaced the patient’s immune system so quickly that the virus had no “reservoirs” left to hide in.
- Heterozygous Advantage: While the donor cells weren’t fully resistant, the single mutation might have slowed the virus down enough for the new immune system to finish the job.
Is This a Cure for Everyone?
While the results are historic, experts urge caution. Stem cell transplants are high-risk procedures with significant mortality rates, typically reserved for patients with terminal blood cancers.
“We shouldn’t forget that 10 years ago, this man had a very high chance of dying from cancer,” says Gaebler. “Today, he has beaten both a deadly cancer and a chronic virus.”
For the vast majority of the 39 million people living with HIV worldwide, standard ART remains the safest and most effective treatment. However, this case provides a vital roadmap for researchers working on gene therapies. If we don’t need a perfect genetic match to achieve a cure, the door opens wider for gene-editing technologies like CRISPR to replicate these results without the need for risky transplants.
The Global Tally
This patient joins an elite group of individuals—including the famous “Berlin Patient” (Timothy Ray Brown) and the “London Patient”—who have shown the world that HIV is not necessarily a life sentence. With over seven years of remission, he currently holds the second-longest record of being virus-free among the seven cured individuals.
Article: Sustained HIV-1 remission after heterozygous CCR5Δ32 stem cell transplantation
https://www.nature.com/articles/s41586-025-09893-0

