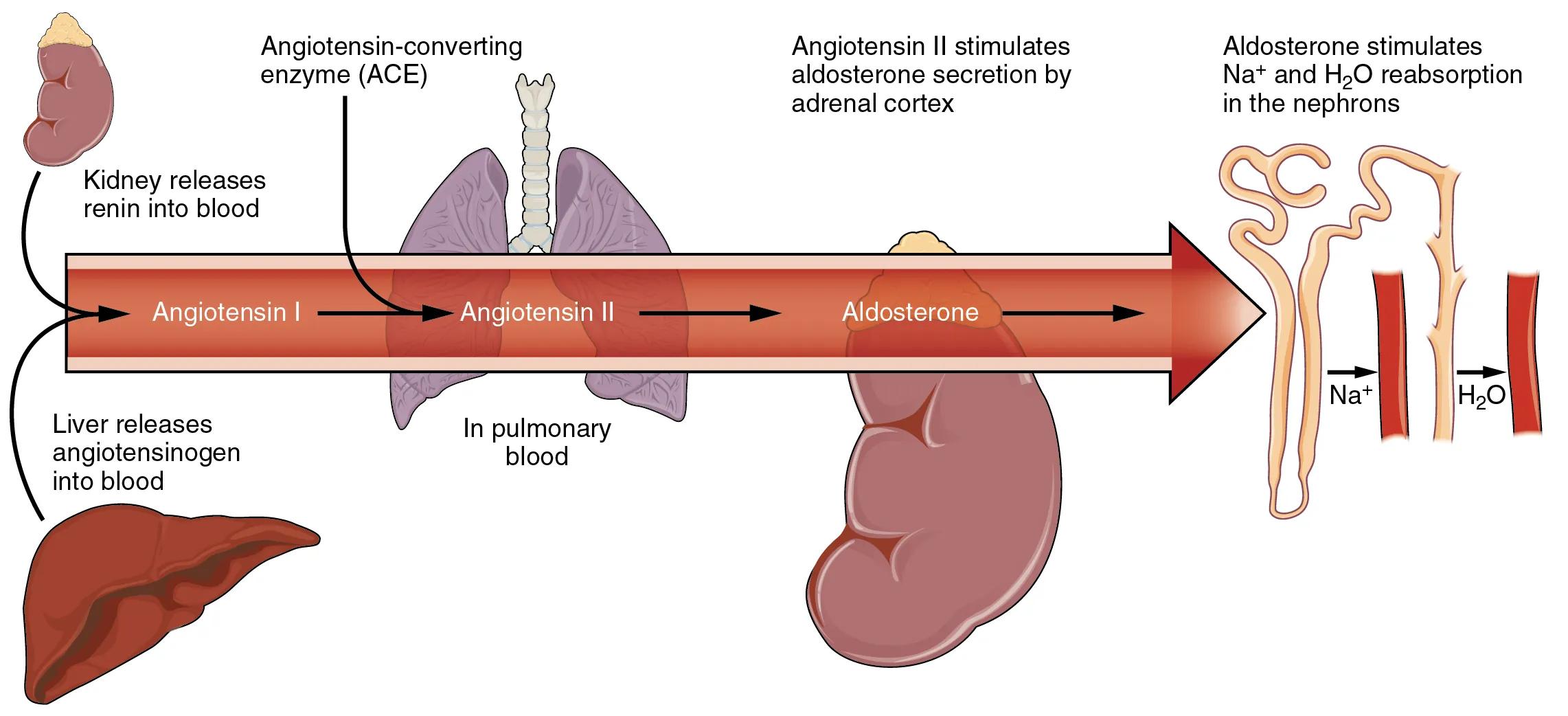
The Renin-Angiotensin System (RAS), also known as the Renin-Angiotensin-Aldosterone System (RAAS), is a critically important hormonal cascade that regulates blood pressure, fluid balance, and electrolyte homeostasis. This diagram visually outlines the key components and sequential activation of the RAS, from the initial release of renin by the kidneys to the final actions of angiotensin II and aldosterone on the body. Understanding this system is fundamental to grasping the pathophysiology of hypertension and various kidney disorders.
Decoding the Renin-Angiotensin System
Kidney releases renin into blood: The kidneys, specifically specialized cells in the juxtaglomerular apparatus, initiate the RAS by releasing the enzyme renin into the bloodstream. This release is primarily stimulated by factors such as a decrease in blood pressure, reduced blood volume, or sympathetic nervous system activity.
Liver releases angiotensinogen into blood: The liver continuously produces and releases a plasma protein called angiotensinogen into the circulation. Angiotensinogen is the precursor to the angiotensins and serves as the substrate upon which renin acts.
Angiotensin I: This is a relatively inactive decapeptide formed in the bloodstream when renin cleaves angiotensinogen. Angiotensin I circulates throughout the body, awaiting further enzymatic conversion to its more active form.
Angiotensin-converting enzyme (ACE): This enzyme is predominantly found in the endothelial cells of the pulmonary (lung) circulation, but also in other tissues. ACE is responsible for converting the inactive angiotensin I into the highly active angiotensin II.
Angiotensin II: This octapeptide is the primary biologically active molecule of the RAS, with widespread and potent effects on the cardiovascular system and fluid balance. It is a powerful vasoconstrictor and a key stimulator of aldosterone release.
In pulmonary blood: This label indicates that a significant portion of the conversion of angiotensin I to angiotensin II by ACE occurs as blood passes through the capillary beds of the lungs. The lungs are rich in ACE, facilitating this crucial step.
Angiotensin II stimulates aldosterone secretion by adrenal cortex: One of the major effects of angiotensin II is to act directly on the adrenal cortex, stimulating it to release aldosterone. This hormonal link is a critical component of the broader Renin-Angiotensin-Aldosterone System.
Aldosterone: This is a steroid hormone released from the adrenal cortex, primarily stimulated by angiotensin II and elevated potassium levels. Aldosterone plays a crucial role in sodium and potassium balance and, consequently, fluid volume.
Aldosterone stimulates Na+ and H2O reabsorption in the nephrons: Aldosterone’s actions in the kidneys, specifically in the distal convoluted tubule and collecting duct of the nephrons, promote the reabsorption of sodium ions. This sodium reabsorption is then followed by the osmotic reabsorption of water, increasing blood volume and contributing to blood pressure regulation.
The Cascade of the Renin-Angiotensin System
The Renin-Angiotensin System (RAS) is a complex yet elegantly designed hormonal axis that plays a pivotal role in the long-term regulation of arterial blood pressure, extracellular fluid volume, and electrolyte balance. Its activation is typically a response to a decrease in renal perfusion pressure (blood flow to the kidneys) or a reduction in sodium delivery to the distal tubules. This initiates a cascade of events involving multiple organs and hormones, ultimately aiming to restore hemodynamic stability.
The initial step involves the kidneys, which release the enzyme renin into the bloodstream in response to specific stimuli. Simultaneously, the liver continuously produces angiotensinogen, a relatively inert precursor protein. Renin then acts upon angiotensinogen, cleaving it to form angiotensin I, a decapeptide that has minimal biological activity on its own.
- The conversion of angiotensin I to its highly potent form, angiotensin II, is catalyzed by Angiotensin-Converting Enzyme (ACE). While ACE is found in many tissues, it is particularly abundant in the endothelial cells lining the blood vessels of the lungs, making the pulmonary circulation a primary site for this conversion.
Angiotensin II is the effector molecule of the RAS, exerting a wide array of physiological effects. It is a powerful vasoconstrictor, directly increasing total peripheral resistance and thereby elevating blood pressure. Furthermore, angiotensin II stimulates the adrenal cortex to release aldosterone, a mineralocorticoid hormone. Aldosterone, in turn, acts on the kidneys to enhance sodium and water reabsorption, leading to an increase in blood volume. The combined effects of vasoconstriction and increased blood volume significantly contribute to the restoration of blood pressure and fluid balance.
Clinical Implications and Therapeutic Targets
The profound influence of the Renin-Angiotensin System on blood pressure and fluid balance makes it a critical target for pharmacological interventions, particularly in the management of hypertension and heart failure. Medications such as ACE inhibitors block the conversion of angiotensin I to angiotensin II, while Angiotensin Receptor Blockers (ARBs) prevent angiotensin II from binding to its receptors. Both classes of drugs effectively attenuate the vasoconstrictive and aldosterone-stimulating effects of angiotensin II, leading to reduced blood pressure and improved cardiovascular outcomes. Understanding the intricacies of the RAS, as depicted in this diagram, is therefore indispensable for healthcare professionals in managing a wide range of cardiovascular and renal conditions.
The Renin-Angiotensin System: A Vital Homeostatic Pathway
The Renin-Angiotensin System (RAS), often expanded to the Renin-Angiotensin-Aldosterone System (RAAS), represents one of the body’s most crucial and sophisticated hormonal pathways for regulating cardiovascular function and fluid-electrolyte balance. Activated primarily in response to conditions like low blood pressure, decreased blood volume, or reduced sodium levels, this system orchestrates a series of physiological responses aimed at restoring homeostasis. Its intricate cascade involves enzymes, peptide hormones, and steroid hormones acting on multiple organs.
The process initiates in the kidney, where specialized cells in the juxtaglomerular apparatus detect changes in renal perfusion or sodium delivery. In response, these cells release the enzyme renin into the bloodstream. Concurrently, the liver continuously synthesizes and secretes angiotensinogen, a plasma alpha-2 globulin, which serves as the substrate for renin. Renin cleaves angiotensinogen to produce angiotensin I, a decapeptide that possesses minimal biological activity on its own. This initial step is rate-limiting for the entire system.
The conversion of the relatively inactive angiotensin I to the potent octapeptide, angiotensin II, is facilitated by Angiotensin-Converting Enzyme (ACE). While ACE is expressed in various tissues, it is particularly abundant in the endothelial cells of the pulmonary vasculature, allowing for efficient conversion as blood passes through the lungs. Angiotensin II then acts as the primary effector molecule of the RAS, mediating several crucial physiological responses. It is a powerful vasoconstrictor, directly elevating systemic vascular resistance and thereby increasing blood pressure. Furthermore, angiotensin II directly stimulates the adrenal cortex to synthesize and release aldosterone, which acts on the kidneys to promote sodium and water reabsorption while enhancing potassium excretion. This combined action of vasoconstriction and fluid retention effectively raises blood volume and blood pressure, counteracting the initial stimuli that triggered the system’s activation.

