The kidneys are master filters of the body, and their efficiency hinges on a highly specialized and intricate vascular system. This article meticulously details the blood flow in the kidney, from the major renal artery entering the organ to the delicate capillary networks where filtration and reabsorption occur. Understanding this sophisticated vascular architecture is paramount to grasping how the kidneys maintain homeostasis and what can go wrong in renal diseases.
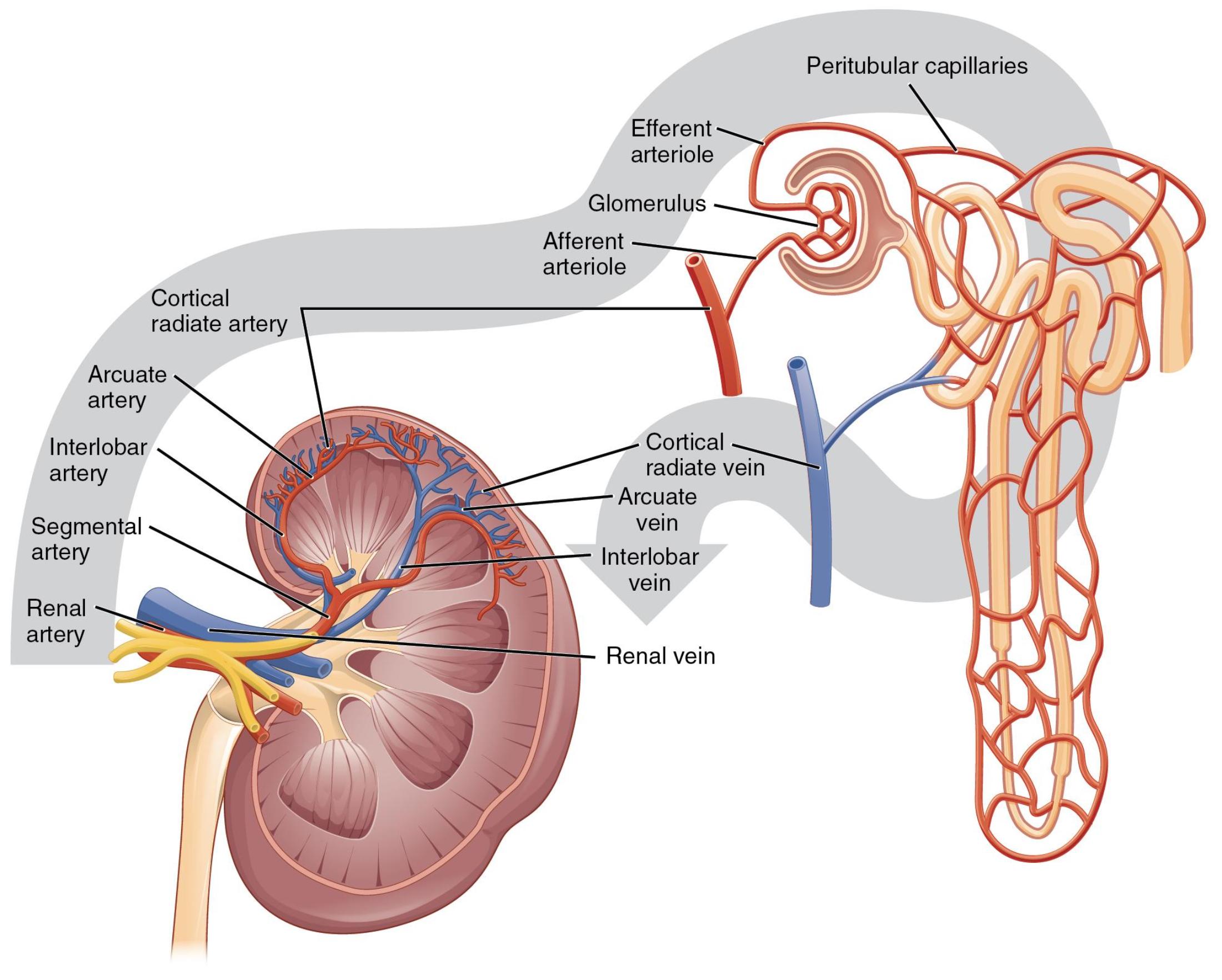
Renal artery: This large artery branches directly from the aorta and is the primary vessel delivering oxygenated, unfiltered blood to the kidney. It typically enters the kidney at the renal hilum.
Segmental artery: The renal artery divides into several segmental arteries as it enters the kidney. Each segmental artery supplies a specific region or segment of the kidney.
Interlobar artery: These arteries branch from the segmental arteries and travel between the renal pyramids within the renal columns. They extend towards the renal cortex.
Arcuate artery: These arteries branch from the interlobar arteries and arch over the bases of the renal pyramids, at the junction of the cortex and medulla. They give rise to smaller arteries that supply the cortex.
Cortical radiate artery (also known as interlobular artery): These small arteries branch off the arcuate arteries and extend into the renal cortex. They give rise to the afferent arterioles, which lead to the glomeruli.
Afferent arteriole: This is a small artery that branches from a cortical radiate artery and carries blood into the glomerulus. Its diameter plays a critical role in regulating glomerular filtration pressure.
Glomerulus: This is a capillary tuft located within Bowman’s capsule, forming the site of initial blood filtration in the kidney. It is a key component of the renal corpuscle, where filtrate is formed.
Efferent arteriole: This small artery carries blood away from the glomerulus, after filtration has occurred. It is narrower than the afferent arteriole, contributing to the high pressure within the glomerulus.
Peritubular capillaries: These are a network of capillaries that surround the renal tubules in the cortex. They reabsorb water and solutes from the filtrate and secrete waste products into it.
Cortical radiate vein: These small veins collect blood from the peritubular capillaries in the cortex. They drain into the arcuate veins.
Arcuate vein: These veins are located at the corticomedullary junction, running parallel to the arcuate arteries. They collect blood from the cortical radiate veins and drain into the interlobar veins.
Interlobar vein: These veins run between the renal pyramids, parallel to the interlobar arteries. They collect blood from the arcuate veins and merge to form the renal vein.
Renal vein: This large vein collects filtered blood from the entire kidney and drains it into the inferior vena cava. It carries blood that has been cleansed of waste products.
The kidneys are highly vascular organs, receiving a substantial portion of the body’s cardiac output—approximately 20-25% at rest. This immense blood supply is critical for their primary function: filtering waste products from the blood to form urine and maintaining the body’s fluid and electrolyte balance. The intricate network of arteries, arterioles, capillaries, and veins ensures that every drop of blood is processed efficiently, highlighting the sophisticated design of the renal system. This image beautifully illustrates the hierarchical branching of blood vessels, providing a clear pathway of blood flow through the kidney’s cortical and medullary regions.
The journey of blood through the kidney begins with the renal artery and culminates with the renal vein, but the processes occurring in between are what make the kidney truly remarkable.
- Filtration: In the glomerulus, a high-pressure capillary bed, plasma is forced out of the blood vessels, forming a protein-free filtrate. This initial step is purely based on size and pressure.
- Reabsorption and Secretion: As the filtrate travels through the renal tubules, essential substances like glucose, amino acids, and most of the water are reabsorbed back into the blood, primarily through the peritubular capillaries. Simultaneously, additional waste products are actively secreted from the blood into the tubules.
This carefully orchestrated flow allows for continuous monitoring and adjustment of blood composition. The unique arrangement of the afferent and efferent arterioles is pivotal in maintaining the high hydrostatic pressure within the glomerulus, driving the filtration process. The narrower efferent arteriole creates resistance, ensuring that blood pressure remains elevated within the glomerular capillaries, even as blood is flowing through them. This pressure gradient is essential for forcing fluid and small solutes out of the blood and into Bowman’s capsule, initiating urine formation. Following filtration, the efferent arteriole gives rise to the peritubular capillaries, which intimately surround the renal tubules. This close proximity facilitates the exchange of substances, allowing for the precise reabsorption of useful components and the secretion of waste, ultimately refining the filtrate into urine.
Any disruption to this delicate vascular system can have severe consequences for kidney function. Conditions such as renal artery stenosis, where the renal artery narrows, can significantly reduce blood flow to the kidney, leading to hypertension and impaired filtration. Glomerulonephritis, an inflammation of the glomeruli, directly impacts the filtering capacity, resulting in the leakage of protein and red blood cells into the urine. Furthermore, uncontrolled diabetes and hypertension are major causes of chronic kidney disease, often damaging the intricate capillary networks within the kidney over time. A thorough understanding of renal blood flow pathways is thus indispensable for diagnosing, treating, and managing a wide spectrum of renal diseases, ensuring targeted interventions that can preserve kidney health and overall well-being.

