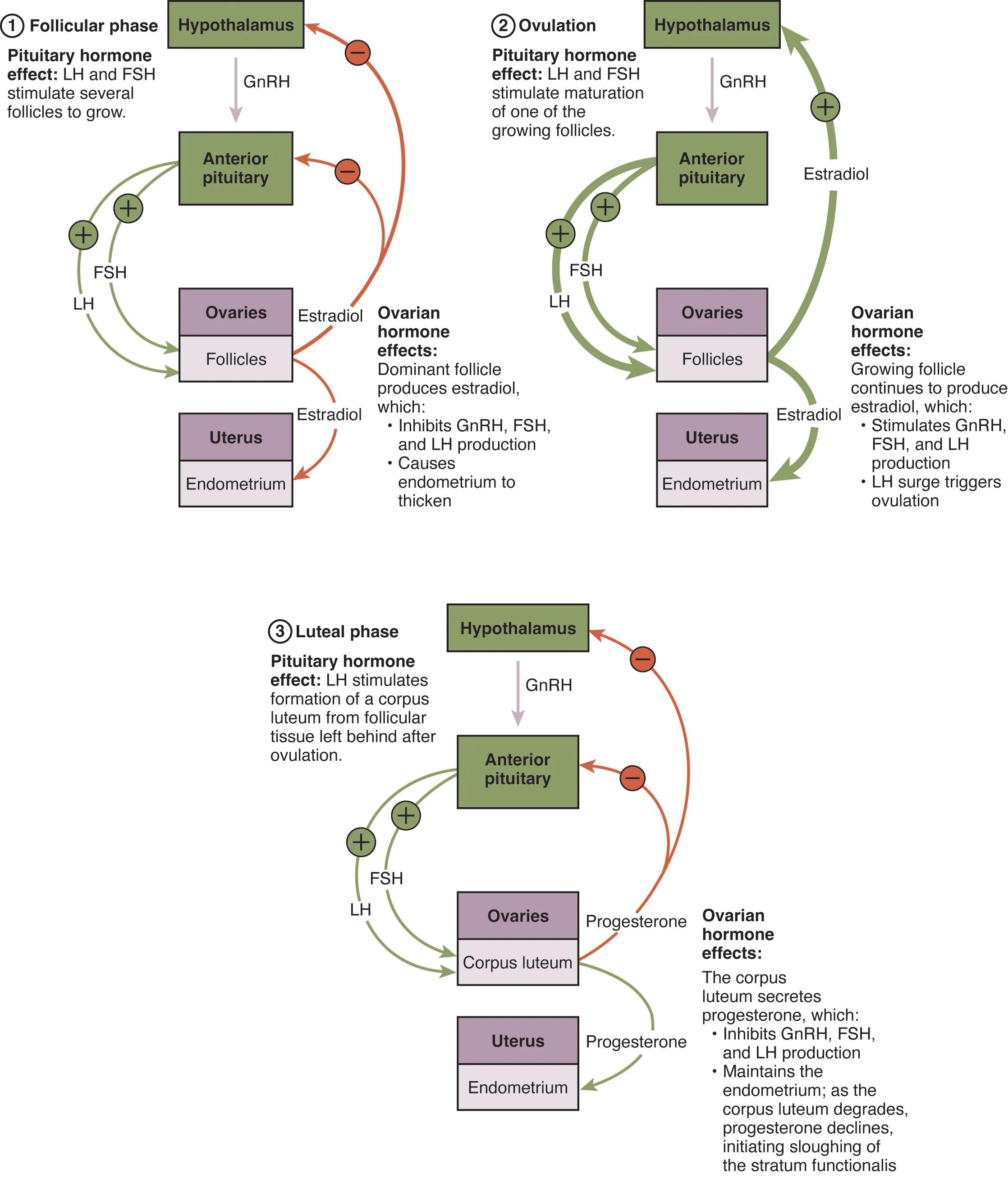
The female reproductive system operates on a finely tuned hormonal cycle, orchestrating ovulation and preparing the uterus for potential pregnancy. This detailed diagram illustrates the intricate interplay between the hypothalamus, pituitary gland, and ovaries, demonstrating how hormones like GnRH, FSH, LH, estradiol, and progesterone regulate the follicular, ovulatory, and luteal phases. Understanding these hormonal dynamics is crucial for comprehending female fertility, menstruation, and reproductive health.
Hypothalamus: The hypothalamus is a vital region of the brain that serves as the command center for many endocrine functions, including the regulation of the ovarian cycle. It releases Gonadotropin-Releasing Hormone (GnRH) in a pulsatile manner, initiating the hormonal cascade.
GnRH: Gonadotropin-Releasing Hormone (GnRH) is a neurohormone produced by the hypothalamus that stimulates the anterior pituitary gland. Its pulsatile release is essential for the proper secretion of FSH and LH, which are critical for ovarian function.
Anterior pituitary: The anterior pituitary is a gland located at the base of the brain, directly stimulated by GnRH from the hypothalamus. In response, it produces and releases Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH), which then act on the ovaries.
FSH: Follicle-Stimulating Hormone (FSH) is a gonadotropin released by the anterior pituitary, primarily responsible for stimulating the growth and development of ovarian follicles. It promotes the proliferation of granulosa cells and estrogen production during the follicular phase.
LH: Luteinizing Hormone (LH) is another gonadotropin from the anterior pituitary, playing multiple crucial roles in the ovarian cycle. It stimulates theca cells to produce androgens, triggers ovulation through a surge, and promotes the formation and function of the corpus luteum.
Ovaries: The ovaries are the primary female reproductive organs, responsible for producing ova (eggs) and secreting key steroid hormones like estradiol and progesterone. They are the target organs for FSH and LH, and their activity defines the ovarian cycle.
Follicles: Ovarian follicles are cellular structures within the ovaries that each contain an oocyte (egg cell) and surrounding supporting cells. They undergo development and maturation throughout the follicular phase, with one typically becoming dominant.
Estradiol: Estradiol is the primary and most potent form of estrogen, produced by the granulosa cells of the developing ovarian follicles under the influence of FSH. High levels of estradiol during the follicular phase stimulate endometrial thickening and, crucially, trigger the LH surge.
Ovarian hormone effects: These refer to the actions of hormones, primarily estradiol and progesterone, produced by the ovaries. These effects include stimulating endometrial growth, and exerting feedback control on the hypothalamus and pituitary to regulate GnRH, FSH, and LH production.
Uterus: The uterus is a hollow, muscular organ in the female pelvis, whose primary function is to house and nourish a developing fetus during pregnancy. Its inner lining, the endometrium, undergoes cyclical changes in response to ovarian hormones.
Endometrium: The endometrium is the inner lining of the uterus, composed of glandular tissue and rich blood supply. It cyclically thickens and prepares for embryo implantation under the influence of estradiol and progesterone, and is shed during menstruation if pregnancy does not occur.
Pituitary hormone effect: LH and FSH stimulate several follicles to grow: During the follicular phase, both LH and FSH from the anterior pituitary act on the ovaries to stimulate the initial growth of a cohort of ovarian follicles. This marks the beginning of the selection process for the dominant follicle.
Ovarian hormone effects: Dominant follicle produces estradiol, which: Inhibits GnRH, FSH, and LH production causes endometrium to thicken: As follicles grow, the dominant follicle increasingly produces estradiol. This estradiol then exerts negative feedback on the hypothalamus (inhibiting GnRH) and anterior pituitary (inhibiting FSH and LH), while also stimulating the uterine endometrium to thicken in preparation for potential implantation.
Pituitary hormone effect: LH and FSH stimulate maturation of one of the growing follicles: Leading up to ovulation, LH and FSH continue to promote the maturation of one selected dominant follicle. This culminates in the follicle becoming ready for the release of its oocyte.
Ovarian hormone effects: Growing follicle continues to produce estradiol, which: Stimulates GnRH, FSH, and LH production. LH surge triggers ovulation: As the dominant follicle matures, its high estradiol production switches from negative to positive feedback, stimulating the hypothalamus to increase GnRH, which in turn leads to a massive surge in LH from the anterior pituitary. This LH surge is the definitive trigger for ovulation.
Pituitary hormone effect: LH stimulates formation of a corpus luteum from follicular tissue left behind after ovulation: After the ovulatory follicle ruptures and releases the oocyte, the remaining follicular cells undergo a transformation under the influence of LH. This results in the formation of the corpus luteum, a temporary but vital endocrine gland.
Ovarian hormone effects: The corpus luteum secretes progesterone, which: Maintains the endometrium; as the corpus luteum degrades, progesterone declines, initiating sloughing of the stratum functionalis: The corpus luteum’s primary function is to secrete progesterone, which is crucial for maintaining the thickened uterine endometrium, making it receptive for embryo implantation. If pregnancy does not occur, the corpus luteum degrades, leading to a drop in progesterone, which causes the functional layer of the endometrium to shed, initiating menstruation.
The Menstrual Cycle: A Symphony of Hormones
The female menstrual cycle is a sophisticated and tightly regulated process, essential for reproduction and overall female health. It represents a continuous interplay between the brain (hypothalamus and pituitary gland) and the ovaries, resulting in cyclical changes in both ovarian follicles (ovarian cycle) and the uterine lining (uterine cycle). This intricate hormonal dance ensures that an egg is released each month and the uterus is prepared for a potential pregnancy. The diagram meticulously dissects the three main phases—follicular, ovulatory, and luteal—highlighting the key hormonal players and their profound effects.
Understanding the sequence and feedback mechanisms of these hormones is fundamental to comprehending not only natural reproductive processes but also the basis for contraceptive methods, fertility treatments, and the diagnosis of various gynecological conditions. The entire system is a prime example of a neuroendocrine loop, where signals from the nervous system are translated into hormonal messages that regulate distant target organs.
Key aspects of hormonal regulation include:
- The pulsatile release of GnRH from the hypothalamus.
- The differential actions of FSH and LH on ovarian follicles.
- The shifting feedback effects of ovarian steroids (estradiol and progesterone) on the brain and pituitary.
- The coordinated preparation of the uterus for potential implantation.
Disruptions in this delicate hormonal balance can lead to irregularities in the menstrual cycle, anovulation, or infertility, emphasizing the importance of this well-tuned physiological system.
Phases of Hormonal Orchestration
The menstrual cycle begins with the follicular phase, where the hypothalamus releases Gonadotropin-Releasing Hormone (GnRH), stimulating the anterior pituitary to secrete Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH). FSH primarily drives the growth of several ovarian follicles, promoting the proliferation of granulosa cells and their production of estradiol. As a dominant follicle emerges, its rising estradiol levels exert negative feedback on the hypothalamus and pituitary, decreasing GnRH, FSH, and LH secretion, thereby preventing the development of other follicles. Concurrently, estradiol acts on the uterus, causing the endometrium to thicken in preparation for a potential embryo.
The rising estradiol levels from the dominant follicle eventually reach a critical threshold, triggering a switch from negative to positive feedback. This leads to a massive surge in LH, known as the LH surge, which marks the beginning of the ovulatory phase. The LH surge is the crucial signal that prompts the mature follicle to rupture, releasing the secondary oocyte from the ovary into the fallopian tube – the event of ovulation. Following ovulation, the remaining cells of the ruptured follicle undergo a dramatic transformation under the influence of LH, developing into the corpus luteum. This structure then initiates the luteal phase, becoming a temporary endocrine gland. The corpus luteum predominantly secretes progesterone, with some estradiol. Progesterone is vital for maintaining the uterine endometrium, making it receptive for embryo implantation. If fertilization and implantation do not occur, the corpus luteum degenerates, leading to a sharp drop in progesterone and estradiol. This hormonal decline causes the functional layer of the endometrium to slough off, resulting in menstruation and marking the start of a new cycle.
In conclusion, the hormonal regulation of the ovarian and uterine cycles is a masterclass in biological coordination, ensuring the precise timing of ovulation and endometrial preparation. The continuous feedback loops involving GnRH, FSH, LH, estradiol, and progesterone are indispensable for female fertility and overall reproductive health. A deep appreciation for these intricate hormonal mechanisms is fundamental for understanding physiological processes, diagnosing reproductive disorders, and developing effective therapeutic strategies.

