Puberty is a transformative period in human development, marked by profound physical and physiological changes that lead to sexual maturity. This intricate process is orchestrated by a delicate balance of hormones, primarily initiated in the brain and culminating in the development of secondary sex characteristics and reproductive capability. Understanding the hormonal cascades involved in puberty is key to appreciating this critical stage of life.
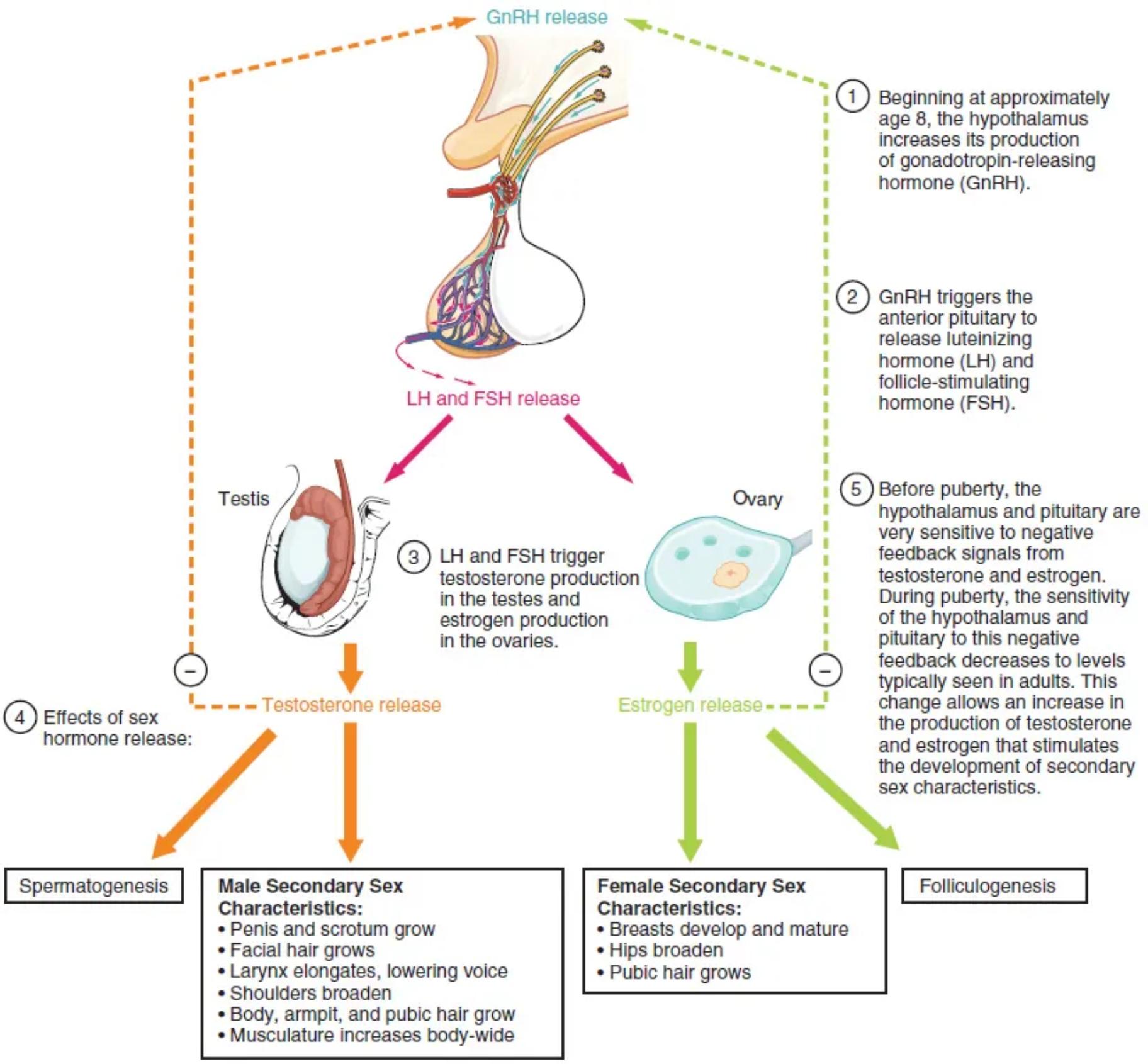
GnRH release: Gonadotropin-releasing hormone (GnRH) is released from the hypothalamus, a region in the brain. This hormone acts as the master switch, initiating the entire cascade of hormonal events that define puberty.
LH and FSH release: Luteinizing hormone (LH) and Follicle-stimulating hormone (FSH) are released from the anterior pituitary gland in response to GnRH. These gonadotropins travel through the bloodstream to the gonads (testes in males, ovaries in females) to stimulate sex hormone production.
Testis: The testes are the primary male reproductive organs, located in the scrotum. Under the influence of LH and FSH, the testes produce testosterone, the main male sex hormone responsible for male secondary sex characteristics and spermatogenesis.
Ovary: The ovaries are the primary female reproductive organs, located in the pelvic cavity. Stimulated by LH and FSH, the ovaries produce estrogen, the main female sex hormone, which drives the development of female secondary sex characteristics and folliculogenesis.
Testosterone release: Testosterone is the principal androgen produced by the testes. Its release is crucial for the development of male secondary sex characteristics, such as deepening of the voice and muscle growth, and for the initiation of sperm production.
Estrogen release: Estrogen is the primary female sex hormone produced by the ovaries. Its release is responsible for the development of female secondary sex characteristics, including breast development and widening of the hips, and for regulating the menstrual cycle.
Spermatogenesis: This is the biological process of producing spermatozoa (sperm cells) in the male testes. It is directly stimulated by testosterone, marking the onset of male fertility.
Male Secondary Sex Characteristics: These are the physical traits that distinguish males from females, apart from the reproductive organs themselves, which develop during puberty. They include changes like penis and scrotum growth, facial and pubic hair growth, and an increase in muscle mass.
Female Secondary Sex Characteristics: These are the physical traits that distinguish females from males, apart from the reproductive organs themselves, which develop during puberty. They include breast development, widening of the hips, and pubic hair growth.
Folliculogenesis: This is the process of ovarian follicle development, which culminates in ovulation. It is stimulated by estrogen and is essential for female reproductive cycles and the potential for conception.
Puberty is a complex biological process that typically begins between the ages of 8 and 14, although the timing can vary significantly among individuals. It is initiated by a series of hormonal changes that transform a child’s body into an adult body capable of reproduction. This period is not merely about physical alterations but also involves significant emotional and psychological development. The hormonal signals originate in the brain, specifically the hypothalamus, and cascade through the pituitary gland to the gonads.
The intricate interplay of hormones ensures that the body develops in a coordinated manner, leading to the acquisition of secondary sex characteristics and the ability to reproduce. Initially, the hypothalamus and pituitary are highly sensitive to the negative feedback from sex hormones. However, as puberty approaches, this sensitivity decreases, allowing for a sustained increase in GnRH, LH, and FSH production.
Key stages of hormonal activation during puberty include:
- Increased GnRH production by the hypothalamus.
- Stimulation of the anterior pituitary to release LH and FSH.
- Activation of the gonads (testes or ovaries) by LH and FSH.
- Production of sex hormones (testosterone or estrogen) by the gonads.
- Development of secondary sex characteristics and reproductive functions.
The onset and progression of puberty are influenced by a combination of genetic, nutritional, and environmental factors. For example, adequate nutrition and body fat percentage are often correlated with the timing of puberty, particularly in females. While the diagram highlights the general pathway, individual experiences of puberty can vary in their exact timeline and intensity.
Understanding the hormonal mechanisms behind puberty is vital for addressing various medical conditions related to growth and sexual development, such as precocious puberty (early onset) or delayed puberty. Medical professionals can intervene when these processes deviate significantly from the typical developmental trajectory, ensuring appropriate health outcomes. The synchronized release and action of these hormones demonstrate a remarkable physiological system designed to prepare the human body for its reproductive years.
In summary, puberty is a remarkable testament to the body’s intricate hormonal regulation, transforming individuals from childhood to reproductive maturity. The orchestrated release of GnRH, LH, FSH, testosterone, and estrogen drives the development of primary and secondary sex characteristics, culminating in the capacity for reproduction. This comprehensive understanding of the hormonal symphony of puberty is essential for both medical professionals and individuals seeking to comprehend this pivotal developmental stage.

