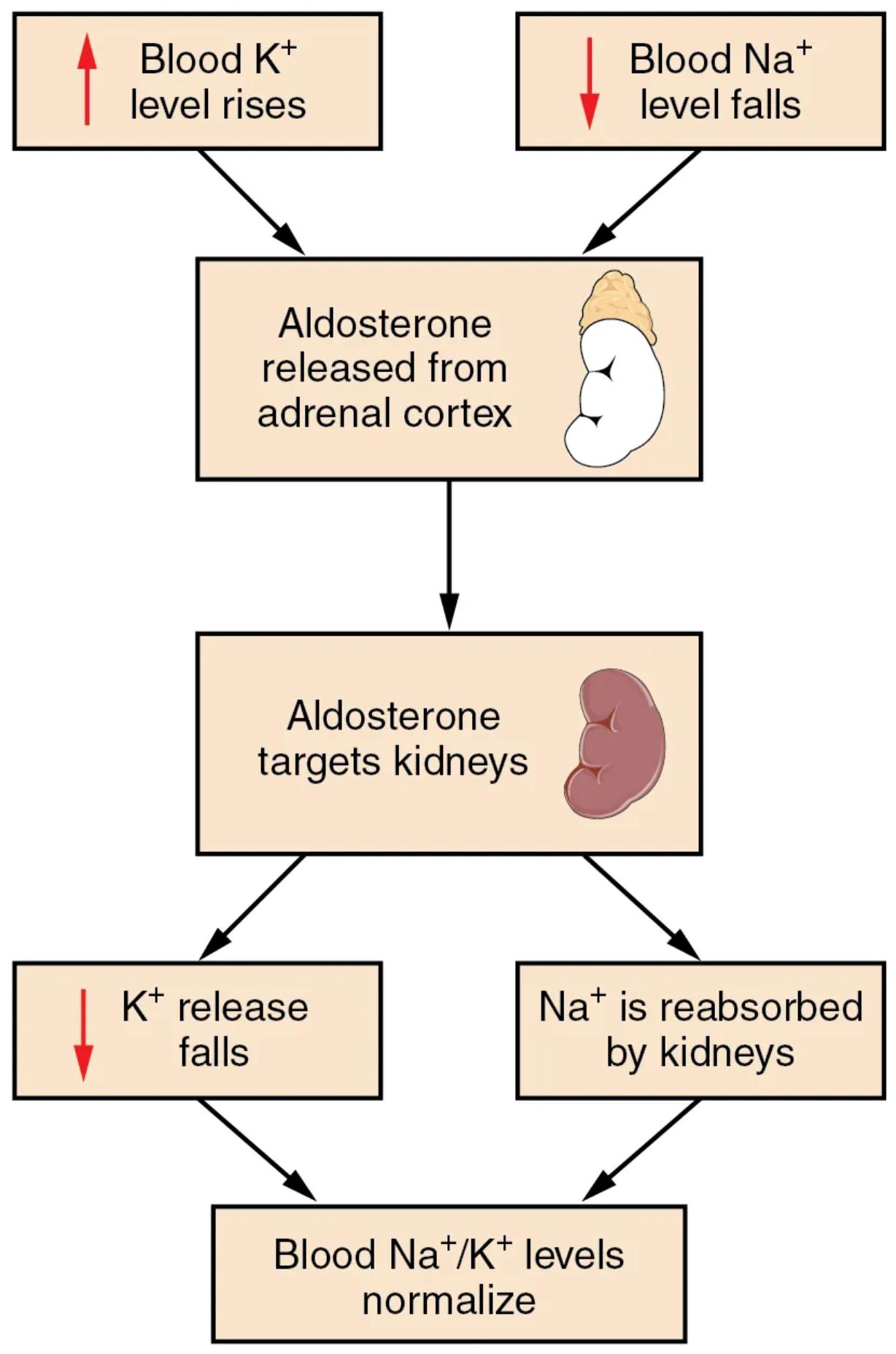
The intricate balance of electrolytes and fluid volume within the body is critical for maintaining overall physiological function. Aldosterone, a powerful steroid hormone, plays a central role in this regulation. This diagram illustrates the aldosterone feedback loop, detailing how fluctuations in blood potassium and sodium levels trigger the release of aldosterone from the adrenal cortex, subsequently acting on the kidneys to restore electrolyte and fluid homeostasis. Understanding this loop is fundamental to comprehending blood pressure control and electrolyte management.
Understanding the Aldosterone Feedback Loop
Blood K+ level rises: An increase in the concentration of potassium ions (K+) in the blood plasma is a direct stimulus for aldosterone release. Maintaining potassium within a narrow range is vital for nerve and muscle function, particularly cardiac muscle.
Blood Na+ level falls: A decrease in the concentration of sodium ions (Na+) in the blood plasma also serves as a potent trigger for aldosterone secretion. Sodium is the primary extracellular cation and is crucial for fluid balance and blood pressure regulation.
Aldosterone released from adrenal cortex: The adrenal cortex, the outer layer of the adrenal gland (located atop the kidneys), is the primary site of aldosterone synthesis and release. This steroid hormone belongs to the mineralocorticoid class and plays a key role in electrolyte balance.
Aldosterone targets kidneys: Once released into the bloodstream, aldosterone travels to its primary target organs, the kidneys. Specifically, it acts on the cells of the distal convoluted tubule and collecting duct.
K+ release falls: Aldosterone promotes the secretion of potassium ions into the renal filtrate for excretion. Therefore, when aldosterone is released, it helps to lower elevated blood potassium levels by increasing its elimination from the body.
Na+ is reabsorbed by kidneys: Aldosterone’s most prominent action is to increase the reabsorption of sodium ions from the renal filtrate back into the bloodstream. This process is crucial because sodium reabsorption is typically followed by water reabsorption, thus expanding blood volume and increasing blood pressure.
Blood Na+/K+ levels normalize: The combined effects of increased sodium reabsorption and increased potassium excretion ultimately lead to the normalization of blood sodium and potassium levels. This re-establishes the crucial electrolyte balance, completing the feedback loop.
The Hormonal Orchestration of Fluid and Electrolytes
Aldosterone is a cornerstone of the body’s homeostatic mechanisms, particularly in the management of fluid volume and electrolyte concentrations. Its actions are indispensable for maintaining blood pressure and preventing dangerous imbalances of sodium and potassium, both of which are vital for cellular function. The release of aldosterone is tightly regulated, ensuring a prompt and appropriate response to deviations from normal electrolyte levels.
The two primary stimuli for aldosterone secretion are directly linked to plasma electrolyte concentrations:
- An increase in blood K+ level (hyperkalemia)
- A decrease in blood Na+ level (hyponatremia)
While these are potent direct stimuli, aldosterone release is also influenced by the renin-angiotensin-aldosterone system (RAAS), which is primarily activated by a drop in blood pressure or blood volume. The adrenal cortex, specifically the zona glomerulosa, acts as the vigilant sensor and producer of this essential hormone.
Upon its release, aldosterone circulates to its main target, the kidneys. Here, it exerts its effects on the epithelial cells of the distal convoluted tubules and collecting ducts. Its principal action is to enhance the activity of sodium-potassium pumps and epithelial sodium channels (ENaCs) on these cells. This leads to increased reabsorption of Na+ from the filtrate back into the bloodstream, often followed by water reabsorption due to osmosis. Concurrently, aldosterone promotes the secretion of K+ into the filtrate for excretion. This dual action effectively corrects the initial electrolyte imbalances, bringing blood Na+/K+ levels back to their physiological set points and influencing overall fluid balance.
Clinical Significance of Aldosterone Regulation
Dysregulation of the aldosterone feedback loop can lead to significant health consequences. For instance, primary hyperaldosteronism (Conn’s syndrome) results from excessive aldosterone production, often by an adrenal adenoma. This leads to increased sodium reabsorption, expanded blood volume, hypertension (high blood pressure), and increased potassium excretion, which can cause hypokalemia. Conversely, conditions like Addison’s disease, characterized by adrenal insufficiency, result in inadequate aldosterone production, leading to sodium loss, hyperkalemia, and potentially life-threatening hypotension. Therefore, a thorough understanding of aldosterone’s actions and its regulatory mechanisms is critical for diagnosing and managing a spectrum of endocrine and cardiovascular disorders.
Aldosterone: A Master Regulator of Sodium and Potassium
The integrity of cellular function, nerve conduction, muscle contraction, and overall blood volume are critically dependent on the precise concentrations of sodium (Na+) and potassium (K+) ions in the extracellular fluid. Aldosterone, a mineralocorticoid hormone synthesized and released by the adrenal cortex, is the principal regulator of these vital electrolytes. This intricate feedback loop ensures that the body maintains a delicate equilibrium, swiftly responding to any imbalances that could compromise physiological stability.
The stimulus for aldosterone secretion primarily arises from two key electrolyte disturbances. First, a rise in blood potassium concentration (hyperkalemia) directly stimulates the cells of the adrenal cortex to release aldosterone. This is a crucial protective mechanism, as elevated potassium levels can disrupt cardiac rhythm and nerve function. Second, a fall in blood sodium concentration (hyponatremia), which often accompanies a decrease in extracellular fluid volume, also triggers aldosterone release. These precise triggers highlight the body’s sophisticated sensing capabilities for maintaining electrolyte homeostasis.
Once released, aldosterone travels through the bloodstream to its target cells, predominantly in the distal convoluted tubules and collecting ducts of the kidneys. Here, it upregulates the synthesis and activity of specific ion channels and pumps, notably the epithelial sodium channels (ENaCs) and the Na+/K+-ATPase pumps. This molecular action leads to a significant increase in the reabsorption of Na+ from the tubular fluid back into the blood. Simultaneously, it promotes the secretion of K+ from the blood into the tubular fluid, facilitating its excretion in urine. The net effect of these actions is a restoration of normal blood Na+ and K+ levels, often accompanied by an increase in water reabsorption due to the osmotic movement of water following sodium, thereby impacting blood volume and pressure. This powerful hormonal control underscores its indispensable role in cardiorenal physiology.

