This article provides a comprehensive overview of spermatogenesis and the anatomical structure of the seminiferous tubule, crucial components of the male reproductive system. Understanding these processes and structures is fundamental to comprehending male fertility and related physiological functions. We will delve into the intricate stages of sperm production, from germ cell division to the maturation of spermatozoa, and explore the cellular architecture that supports this vital biological process.
Anatomical Labels and Explanations:
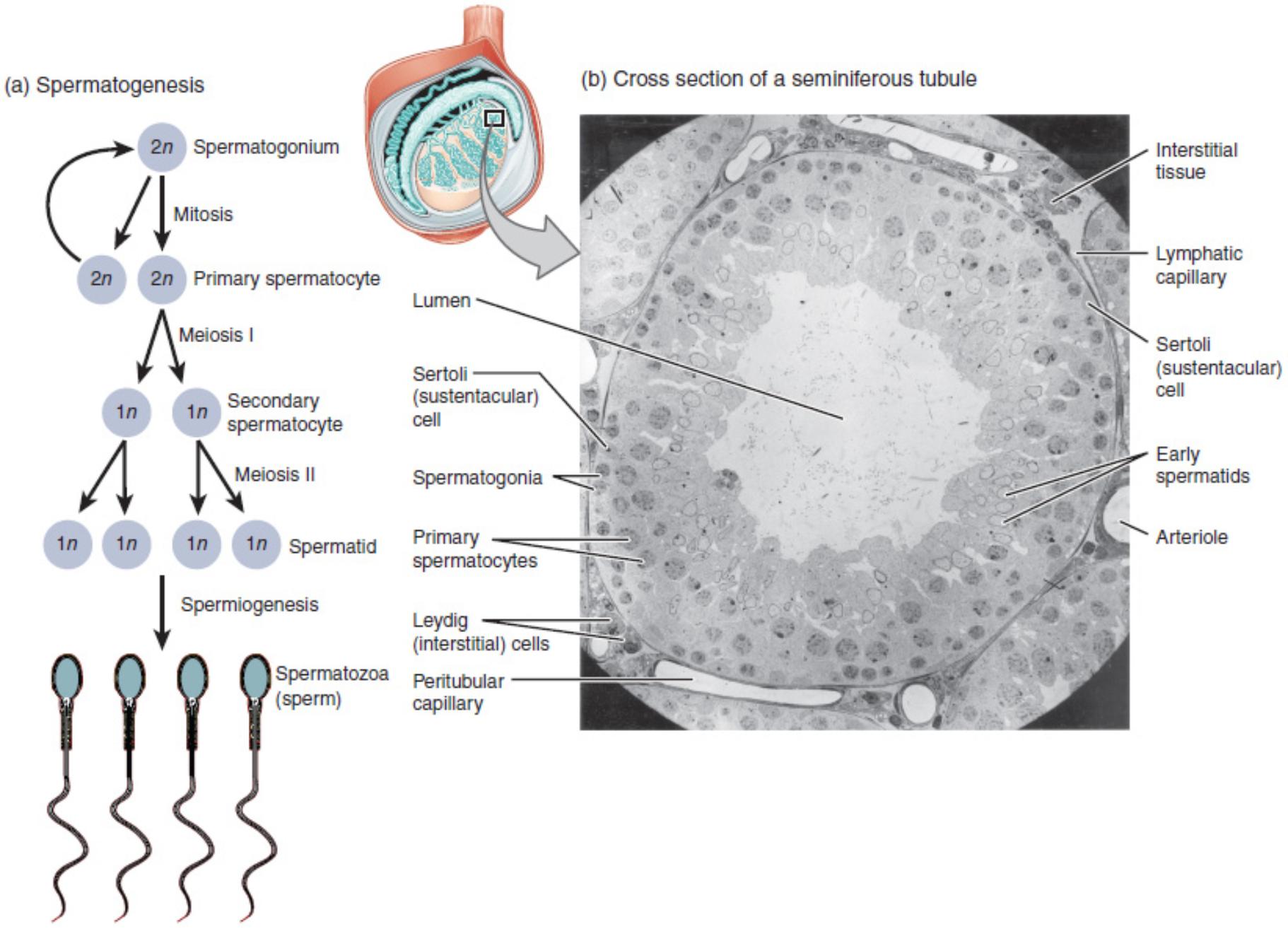
Interstitial tissue: This tissue surrounds the seminiferous tubules within the testes. It contains various cell types, including Leydig cells, which are responsible for producing testosterone.
Lymphatic capillary: These small vessels are part of the lymphatic system, which plays a role in fluid balance and immune surveillance. They are found within the interstitial tissue, helping to drain excess fluid and transport immune cells.
Sertoli (sustentacular) cell: These large, columnar cells extend from the basement membrane to the lumen of the seminiferous tubule. They provide structural support and nourishment to developing germ cells, forming the blood-testis barrier and secreting various factors essential for spermatogenesis.
Early spermatids: These are immature male gametes that have completed meiosis II and are undergoing spermiogenesis. They are located closer to the lumen of the seminiferous tubule and are characterized by their developing flagella.
Arteriole: A small artery that branches into capillaries, providing oxygenated blood and nutrients to the cells within the seminiferous tubule and surrounding interstitial tissue.
Lumen: This is the central, open space within the seminiferous tubule. Mature spermatozoa are released into the lumen before being transported out of the testes.
Spermatogonia: These are diploid germ cells located at the base of the seminiferous tubule, near the basement membrane. They are stem cells that undergo mitosis to produce more spermatogonia and primary spermatocytes, initiating the process of spermatogenesis.
Primary spermatocytes: These are diploid cells that have entered meiosis I. They are larger than spermatogonia and are found slightly further from the basement membrane within the seminiferous tubule.
Leydig (interstitial) cells: Located in the interstitial tissue between the seminiferous tubules, these endocrine cells are responsible for synthesizing and secreting androgens, primarily testosterone, which is crucial for male sexual development and spermatogenesis.
Peritubular capillary: These tiny blood vessels surround the seminiferous tubules. They facilitate the exchange of nutrients, oxygen, and waste products between the blood and the cells within the tubules, including the developing sperm cells.
Spermatogenesis: The Journey of Sperm Formation
The process of spermatogenesis, depicted in part (a) of the image, is a highly regulated and continuous process that produces mature sperm cells. It begins with spermatogonia, diploid stem cells located at the periphery of the seminiferous tubules. These cells undergo mitotic division, ensuring a continuous supply of germ cells. Some spermatogonia differentiate into primary spermatocytes, which then enter meiosis I.
Meiosis I is a crucial stage where homologous chromosomes pair and exchange genetic material, leading to genetic diversity. Each primary spermatocyte divides into two haploid secondary spermatocytes. These secondary spermatocytes quickly proceed to meiosis II, resulting in four haploid spermatids from each primary spermatocyte. These spermatids are still immature and undergo a final transformative phase called spermiogenesis.
During spermiogenesis, spermatids undergo significant morphological changes, including the formation of a head containing the nucleus, a midpiece packed with mitochondria for energy, and a flagellum for motility. This intricate process transforms the round spermatid into the streamlined, motile spermatozoa (sperm), ready for fertilization. The entire process of spermatogenesis takes approximately 64 days in humans, highlighting its complex and time-consuming nature.
Part (b) of the image provides a detailed electron micrograph of a cross-section of a seminiferous tubule, illustrating the organized arrangement of cells involved in spermatogenesis. The lumen, the central light-shaded area, is where mature sperm are released. The progression of germ cell development can be observed from the basement membrane, where spermatogonia reside, towards the lumen, where early spermatids are found. This spatial arrangement reflects the chronological order of spermatogenesis, with various cell types at different stages of development strategically positioned within the tubule.
The supportive role of Sertoli cells is paramount in this environment. These cells not only provide physical support but also create a microenvironment essential for germ cell differentiation and maturation, including the formation of the blood-testis barrier which protects developing sperm from immune attack. The surrounding interstitial tissue, containing Leydig cells and a rich vascular supply, further emphasizes the complex interplay of cellular and hormonal factors that drive successful spermatogenesis.
Conclusion
In summary, spermatogenesis is a remarkable biological process that ensures the continuous production of male gametes, crucial for reproduction. The intricate interplay between germ cells, supportive Sertoli cells, and hormone-producing Leydig cells within the highly organized structure of the seminiferous tubules underscores the complexity and efficiency of the male reproductive system. Understanding these fundamental aspects is vital for appreciating the delicate balance required for male fertility and diagnosing potential disruptions in this essential process.

