This article provides a comprehensive overview of spermatogenesis, the intricate biological process of sperm formation, as illustrated by the accompanying diagram. Understanding the stages of spermatogenesis is fundamental to comprehending male reproductive biology and the mechanisms underlying male fertility. We will delineate each critical phase, from germ cell proliferation through meiosis to the final maturation of spermatozoa, highlighting the genetic transformations and morphological changes that occur.
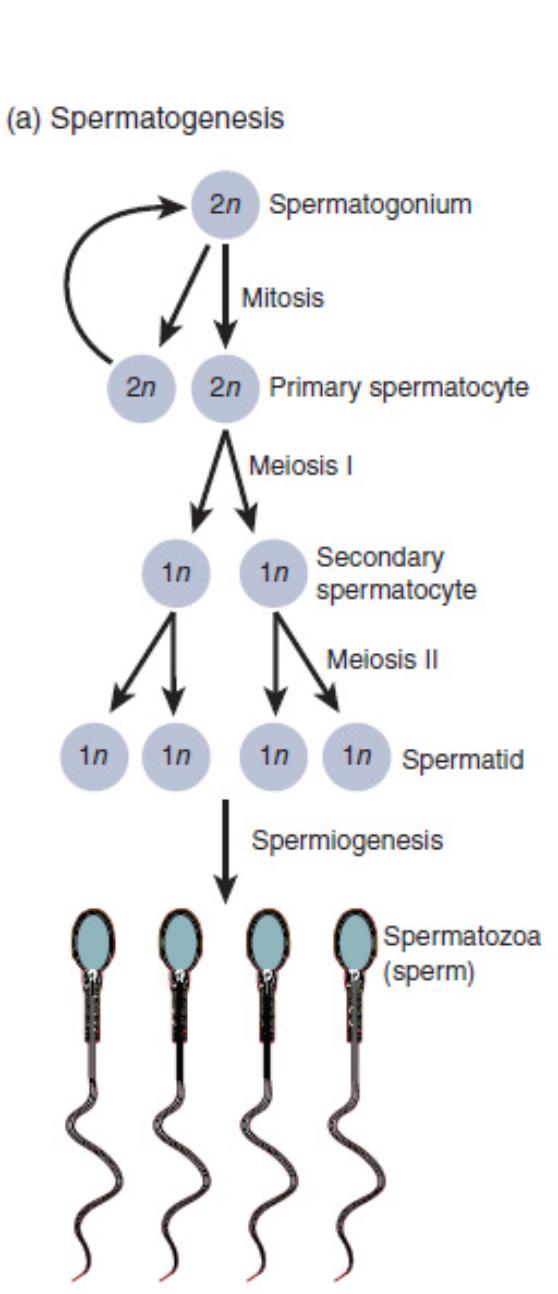
Diagram Labels and Explanations:
Spermatogonium (2n): These are diploid (2n) germline stem cells located in the seminiferous tubules of the testes. They serve as the progenitor cells for all subsequent stages of spermatogenesis, capable of both self-renewal and differentiation.
Mitosis: This is a type of cell division where a single diploid cell divides into two identical diploid daughter cells. In spermatogenesis, spermatogonia undergo mitosis to produce more spermatogonia and to generate primary spermatocytes.
Primary spermatocyte (2n): These are diploid (2n) cells that result from the mitotic division of spermatogonia and subsequently enter meiosis I. They are the largest germ cells in the seminiferous tubule and are committed to producing haploid gametes.
Meiosis I: This is the first round of meiotic division, characterized by the separation of homologous chromosomes. Each primary spermatocyte divides into two haploid secondary spermatocytes, reducing the chromosome number by half.
Secondary spermatocyte (1n): These are haploid (1n) cells formed after Meiosis I from a primary spermatocyte. They are short-lived and rapidly proceed to Meiosis II without an intervening interphase.
Meiosis II: This is the second round of meiotic division, where sister chromatids separate, similar to mitosis. Each secondary spermatocyte divides into two haploid spermatids, resulting in four haploid cells from the original primary spermatocyte.
Spermatid (1n): These are haploid (1n) cells that are the direct products of Meiosis II. While they possess the correct chromosome number, they are still immature and lack the characteristic morphology of mature sperm, particularly their motility.
Spermiogenesis: This is the final stage of spermatogenesis, a post-meiotic maturation process where spermatids differentiate into spermatozoa. It involves significant morphological changes but no further cell division.
Spermatozoa (sperm): These are the mature, haploid male gametes, characterized by a head containing the nucleus, a midpiece rich in mitochondria, and a long flagellum for motility. They are the functional cells capable of fertilizing an ovum.
The Journey of Spermatogenesis: From Germ Cell to Mature Sperm
The diagram vividly illustrates the complex and highly regulated process of spermatogenesis, the biological cascade that produces male gametes. This journey begins with spermatogonia, which are diploid stem cells located in the seminiferous tubules. These foundational cells are crucial for ensuring a continuous supply of germ cells throughout a male’s reproductive life.
The initial phase involves mitosis, where a spermatogonium divides to produce two identical diploid daughter cells. One of these cells may remain a spermatogonium, ensuring self-renewal of the stem cell pool, while the other differentiates into a primary spermatocyte. This primary spermatocyte then embarks on the transformative process of meiosis.
Meiosis is a specialized two-stage cell division that reduces the chromosome number by half and introduces genetic diversity.
- Meiosis I: The primary spermatocyte undergoes this division, separating homologous chromosomes and forming two haploid secondary spermatocytes. This is a critical reductional division.
- Meiosis II: Each secondary spermatocyte rapidly progresses to this second division, separating sister chromatids to yield two haploid spermatids. Consequently, from one primary spermatocyte, four haploid spermatids are produced.
The final crucial stage is spermiogenesis, a period of extensive morphological remodeling. During spermiogenesis, the non-motile, round spermatids are transformed into the highly specialized, motile spermatozoa. This involves the condensation of the nucleus, formation of an acrosome (a cap-like organelle essential for fertilization), development of a midpiece packed with mitochondria for energy, and the growth of a flagellum for propulsion. This intricate process ensures the production of functionally mature sperm capable of fertilization.
Conclusion
The diagram of spermatogenesis elegantly summarizes the sequential stages involved in the production of male gametes. From the initial mitotic proliferation of spermatogonia to the meiotic divisions that generate haploid spermatids, and finally to the dramatic morphological changes of spermiogenesis, each step is essential for creating viable spermatozoa. A thorough understanding of this developmental pathway is indispensable for grasping the fundamental principles of human reproduction and for investigating conditions related to male infertility.

