Delve into the intricate cellular landscape of the small intestinal mucosa, where a diverse array of specialized cells orchestrates digestion, nutrient absorption, and immune defense. This article explores the unique functions of each cell type, from the primary absorptive cells to the enteroendocrine cells that regulate gastrointestinal activity, providing a comprehensive understanding of this vital digestive region.
Absorptive cells: These columnar epithelial cells are the most abundant cell type lining the villi and crypts of the small intestine. Their primary function is the digestion and absorption of nutrients, facilitated by their extensive brush border and rich enzymatic activity.
Goblet cells: Scattered among the absorptive cells, these specialized glandular cells are responsible for secreting mucus. This mucus forms a protective layer, lubricating the intestinal surface and shielding it from mechanical damage and enzymatic degradation.
Paneth cells: Located primarily at the base of the intestinal glands (crypts of Lieberkühn), Paneth cells play a crucial role in innate immunity. They secrete various antimicrobial peptides, including the bactericidal enzyme lysozyme, and are also capable of phagocytosis to defend against pathogens.
G cells: Found within the intestinal glands of the duodenum, G cells are a type of enteroendocrine cell. They secrete the hormone intestinal gastrin, which stimulates gastric acid secretion in the stomach, thus aiding in the initial stages of digestion.
I cells: Also located in the intestinal glands of the duodenum, I cells are another class of enteroendocrine cells. They are responsible for the secretion of the hormone cholecystokinin (CCK), which stimulates the release of pancreatic juices and bile, crucial for fat and protein digestion.
K cells: These enteroendocrine cells are found in the intestinal glands of the small intestine. K cells secrete the hormone glucose-dependent insulinotropic peptide (GIP), which stimulates the release of insulin from the pancreas in response to glucose, thereby playing a role in glucose metabolism.
M cells: Situated in the intestinal glands of the duodenum and jejunum, M cells secrete the hormone motilin. Motilin accelerates gastric emptying, stimulates intestinal peristalsis, and stimulates the production of pepsin, coordinating digestive motility.
S cells: Located in the intestinal glands, S cells are enteroendocrine cells that secrete the hormone secretin. Secretin primarily stimulates the pancreas to release bicarbonate-rich fluid, which neutralizes acidic chyme entering the duodenum and promotes optimal enzyme activity.
The small intestine is a remarkable organ, not only for its vast absorptive surface area but also for the incredible diversity and specialization of its cellular components. The mucosa of the small intestine is a complex tapestry of various cell types, each playing a vital, distinct role in the multifaceted processes of digestion, nutrient absorption, and immune defense. This cellular intricacy underscores the sophisticated mechanisms that ensure our bodies efficiently extract nutrients from food while maintaining a protective barrier against potential threats.
From the primary workhorses of nutrient uptake to the specialized cells that secrete protective mucus, antimicrobial agents, and regulatory hormones, the small intestinal mucosa is a hub of intense biological activity. These cells are not static; they are dynamically regulated, responding to the presence of food, changes in pH, and signals from other parts of the digestive system. Understanding the specific functions of these cellular players provides critical insight into the overall efficiency and resilience of the human digestive tract.
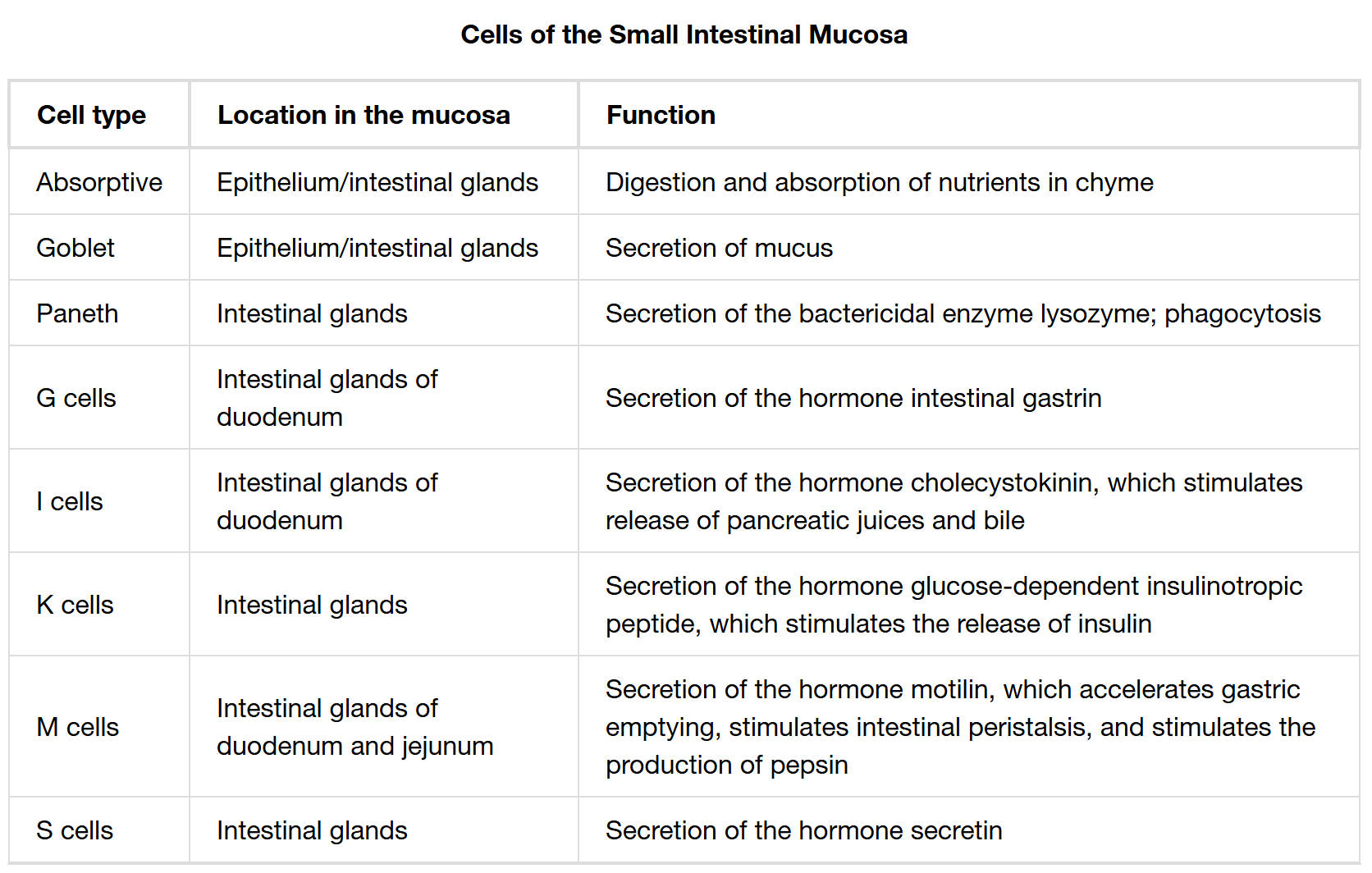
The coordinated efforts of these cells ensure that chyme, the partially digested food from the stomach, is thoroughly broken down into absorbable components, and that these components are then efficiently transported into the bloodstream or lymphatic system. Furthermore, these cells contribute significantly to the local immune environment, safeguarding the body from ingested pathogens. The table above meticulously outlines the specific roles of key cell types found within the small intestinal mucosa, highlighting their location and primary functions.
The small intestinal mucosa is a vibrant ecosystem of specialized cells, each contributing to the organ’s critical functions. The table above provides a concise overview of the major cell types, their locations, and their primary roles in this intricate environment.
Primary Digestive and Protective Cells
- Absorptive cells (Enterocytes): These are the workhorses of the small intestine, forming the vast majority of the epithelial lining. Their apical surfaces are covered with microvilli, creating the brush border which contains enzymes for the final stages of carbohydrate and protein digestion. They are responsible for the active transport of nutrients such as monosaccharides, amino acids, fatty acids, and vitamins into the underlying capillaries and lacteals.
- Goblet cells: Strategically interspersed among the absorptive cells, goblet cells produce and secrete mucin, which hydrates to form a protective layer of mucus. This layer is essential for lubricating the intestinal tract and protecting the delicate epithelial lining from the abrasive action of chyme and the potent digestive enzymes within the lumen.
- Paneth cells: Located deep within the intestinal glands, Paneth cells are key components of the intestinal innate immune system. They secrete antimicrobial peptides, most notably lysozyme, and defensins, which help regulate the microbial population within the small intestine and protect against bacterial invasion. Their phagocytic activity further contributes to immune defense.
Enteroendocrine Cells: Hormonal Regulators
A significant portion of the small intestine’s regulatory capabilities comes from its diverse population of enteroendocrine cells, which act as sensors for luminal contents and release hormones to orchestrate digestive processes:
- G cells: These cells, specifically found in the duodenum, produce intestinal gastrin. While gastrin is more famously associated with the stomach, intestinal gastrin contributes to the overall stimulation of gastric acid secretion, thereby aiding in the initial breakdown of food.
- I cells: Secreting cholecystokinin (CCK), I cells are crucial for fat and protein digestion. CCK stimulates the gallbladder to contract and release bile into the duodenum, which emulsifies fats. It also promotes the release of enzyme-rich pancreatic juices, essential for breaking down all macronutrients.
- K cells: These cells release glucose-dependent insulinotropic peptide (GIP). GIP acts on the pancreas to stimulate insulin release in response to the presence of glucose in the small intestine, linking digestion directly to blood glucose regulation. This “incretin effect” primes the body for glucose uptake.
- M cells: Secreting motilin, M cells play a role in regulating gastrointestinal motility. Motilin initiates the migrating motor complex (MMC) during fasting, which helps sweep undigested material through the small intestine, and also influences gastric emptying and intestinal peristalsis after a meal.
- S cells: These cells are responsible for the secretion of secretin, a hormone vital for neutralizing stomach acid. Secretin stimulates the pancreas to release a bicarbonate-rich fluid into the duodenum, elevating the pH to an optimal range for pancreatic enzyme activity and protecting the duodenal mucosa.
In conclusion, the small intestinal mucosa is far more than just a surface for absorption; it is a highly sophisticated, multi-functional tissue composed of specialized cells that work in harmony. From the primary absorptive cells to the goblet cells providing protection, the immune-defending Paneth cells, and the array of enteroendocrine cells that regulate everything from gastric emptying to insulin release, each cell type plays an indispensable role. This intricate cellular orchestration is fundamental to efficient digestion, robust immune function, and the overall maintenance of gut health, underscoring the vital importance of the small intestine in human physiology.

