Explore the essential process of triglyceride breakdown into monoglycerides and fatty acids, a critical step in fat digestion and absorption. This mechanism allows the body to efficiently utilize dietary fats for energy, storage, and the synthesis of vital compounds.
Understanding the Triglyceride Breakdown Diagram
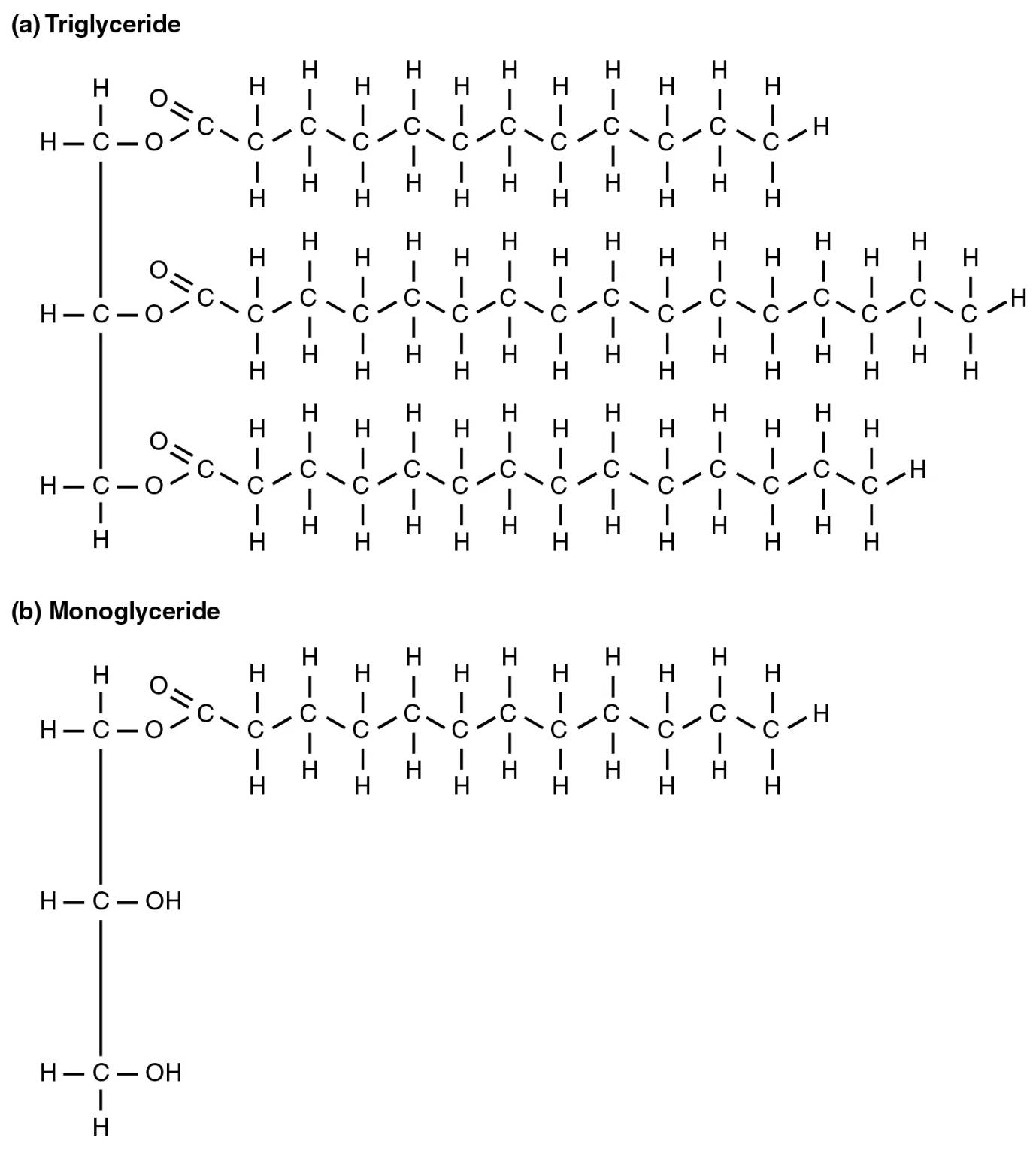
Triglyceride (a): A triglyceride is the most common type of fat found in the body and in most foods. It consists of a glycerol backbone esterified to three fatty acid chains, serving as the primary form of energy storage.
Monoglyceride (b): A monoglyceride is a molecule composed of a glycerol backbone with only one fatty acid chain attached. It is formed during the digestion of triglycerides when two of the three fatty acid chains are removed.
The Dynamics of Dietary Fat Metabolism
Dietary fats, primarily consumed as triglycerides, represent a concentrated source of energy and are crucial for the absorption of fat-soluble vitamins (A, D, E, K). However, due to their hydrophobic nature, triglycerides cannot be directly absorbed into the bloodstream in their intact form. Instead, they must undergo a meticulous process of digestion and breakdown in the gastrointestinal tract, transforming them into smaller, more manageable components that can traverse the intestinal lining. This sophisticated enzymatic hydrolysis is fundamental to our ability to utilize fats for various physiological functions.
The journey of triglyceride digestion begins in the stomach with gastric lipase, but the bulk of the breakdown occurs in the small intestine. Here, bile salts, produced by the liver and stored in the gallbladder, play a critical role in emulsifying large fat globules into smaller droplets. This emulsification significantly increases the surface area for the action of pancreatic lipase, the primary enzyme responsible for triglyceride hydrolysis. Without proper emulsification, pancreatic lipase would be much less efficient, leading to malabsorption of fats.
Pancreatic lipase efficiently cleaves the ester bonds connecting the fatty acids to the glycerol backbone. Specifically, it acts on the fatty acids at the sn-1 and sn-3 positions of the glycerol molecule, typically releasing two free fatty acids and leaving behind a 2-monoglyceride. This breakdown product, along with the liberated free fatty acids, can then be incorporated into mixed micelles. These micelles, stabilized by bile salts, are essential for transporting these hydrophobic digestion products to the surface of the intestinal absorptive cells (enterocytes).
- Triglycerides are the main form of dietary fat.
- Digestion primarily occurs in the small intestine.
- Pancreatic lipase breaks down triglycerides.
- The main products are monoglycerides and free fatty acids.
From Digestion to Cellular Utilization
Upon reaching the enterocytes, the monoglycerides and free fatty acids diffuse across the brush border membrane, leaving the bile salts behind in the intestinal lumen to be reabsorbed and recycled. Once inside the enterocyte, these components are re-esterified back into triglycerides within the endoplasmic reticulum. This re-synthesis is crucial because intact triglycerides are then packaged into chylomicrons, large lipoprotein particles designed for transport.
Chylomicrons, filled with re-synthesized triglycerides, are too large to directly enter the bloodstream. Instead, they are released into the lymphatic system, eventually making their way into the systemic circulation. Once in the bloodstream, chylomicrons deliver their triglyceride cargo to various tissues, particularly adipose tissue for storage and muscle tissue for immediate energy use. This delivery is facilitated by lipoprotein lipase, an enzyme anchored to the walls of capillaries in these tissues, which again hydrolyzes the triglycerides back into free fatty acids and glycerol, allowing them to be taken up by the cells.
The released free fatty acids can then be either oxidized for energy through beta-oxidation, leading to the production of acetyl CoA and subsequently ATP, or re-esterified for storage. Glycerol, the backbone of triglycerides, is transported to the liver, where it can be used for glucose synthesis via gluconeogenesis or re-esterified to form new triglycerides. This dynamic cycle of breakdown, absorption, re-synthesis, and utilization highlights the body’s sophisticated mechanisms for managing its fat resources, ensuring efficient energy supply and storage.
Clinical Implications of Dysfunctional Fat Metabolism
Dysregulation in triglyceride breakdown and metabolism can lead to several significant health issues. High levels of triglycerides in the blood, a condition known as hypertriglyceridemia, are a recognized risk factor for cardiovascular disease. While directly contributing to atherosclerosis is complex, very high triglyceride levels can lead to acute pancreatitis, a severe inflammation of the pancreas. Factors such as diet rich in refined carbohydrates, excessive alcohol consumption, obesity, and certain genetic predispositions can all contribute to elevated triglyceride levels.
Furthermore, conditions that impair fat digestion and absorption, such as exocrine pancreatic insufficiency (e.g., in cystic fibrosis) or diseases affecting bile production (e.g., cholestasis), can lead to fat malabsorption. This results in steatorrhea (fatty stools), deficiencies in fat-soluble vitamins, and overall malnutrition. Medical interventions often involve enzyme replacement therapy or dietary modifications to manage these conditions effectively, underscoring the critical importance of a healthy and functional digestive system for proper fat metabolism.
Conclusion
The breakdown of triglycerides into monoglycerides and free fatty acids is an indispensable step in the intricate process of fat metabolism, facilitating the absorption and utilization of dietary fats. This enzymatic hydrolysis, primarily driven by pancreatic lipase in the small intestine, is crucial for energy provision, nutrient absorption, and maintaining overall physiological balance. A comprehensive understanding of this pathway is vital not only for appreciating the complexities of human digestion but also for addressing metabolic disorders associated with fat malabsorption or dyslipidemia, ultimately contributing to better health outcomes.

