Introduction
This case study presents a diagnostic challenge in a 14-year-old male initially presenting with symptoms suggestive of pneumonia but whose persistent symptoms and subsequent investigations pointed towards a more complex etiology, ultimately leading to a diagnosis of tuberculosis. We will review his clinical course, imaging findings, and management.
Patient Presentation
A 14-year-old male, with no known chronic illnesses or regular medications, was referred to the emergency department with a presumptive diagnosis of pneumonia. His symptoms, which began 10 days prior, included fever, malaise, and cough. He had initially presented to an emergency department where he was prescribed antibiotics. Due to persistent symptoms, he was referred to our center. After a 2-day observation period, he was prescribed intravenous antibiotics to be administered daily, followed by oral antibiotics. Despite reportedly adhering to his medication regimen, his symptoms did not resolve, prompting a follow-up visit to the outpatient clinic.
Upon re-evaluation in the emergency department, physical examination revealed crackles in the right upper lobe. He was not desaturated and had no increased respiratory effort. He had no history of nebulizer use or hospitalizations for respiratory issues, and this was his first such presentation. Blood tests and imaging studies were performed. He was admitted to the pediatric health and diseases service for further investigation and treatment with preliminary diagnoses of pneumonia and tuberculosis.
Relevant Medical History:
- A reaction developed after vancomycin treatment during observation.
- No known history of tuberculosis in either parent.
- Mother has diabetes, and father has inflammatory joint rheumatism.
Clinical Course on Day 7 of Hospitalization for Tuberculosis
On the seventh day of hospitalization for tuberculosis, the patient’s general condition was moderate. He experienced intermittent fevers and nausea, but other vital signs remained stable.
Physical Examination (Day 7):
- Respiratory System: Decreased breath sounds and crackles were noted in the right upper zone. He was monitored on room air and was not desaturated.
- Symptoms: Malaise, loss of appetite, and cough persisted, with no additional complaints.
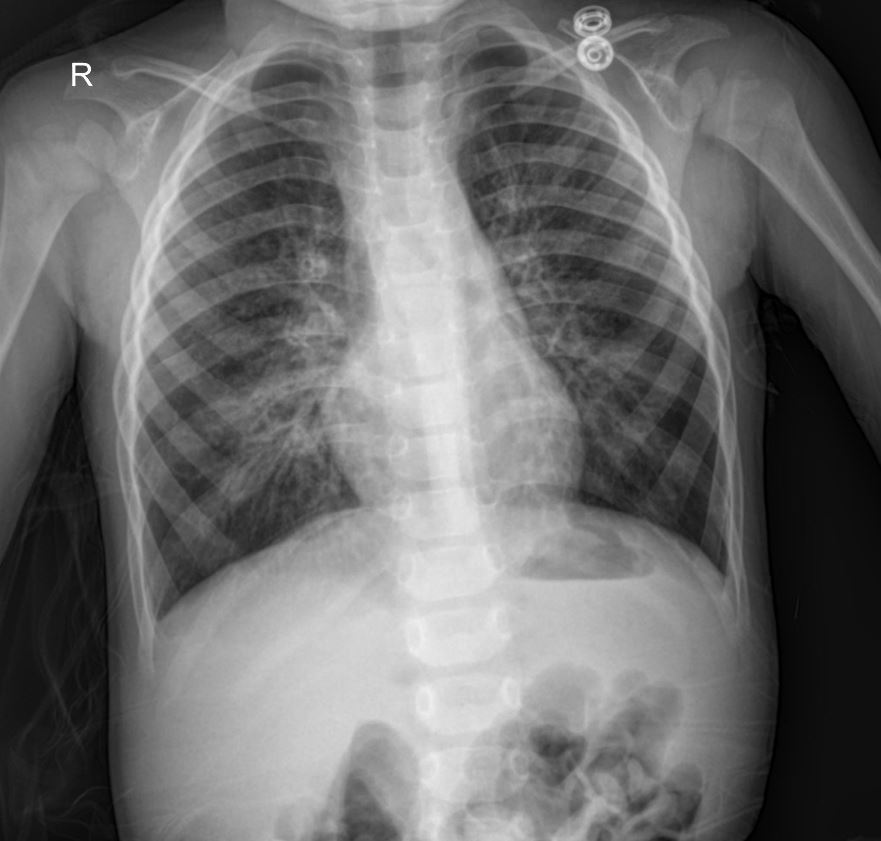
Chest X-Ray Findings
The initial chest X-ray revealed significant infiltrates in the right upper lobe, consistent with a consolidative process. The findings raised suspicion for a bacterial pneumonia, but given the lack of response to broad-spectrum antibiotics and the clinical context, other possibilities, including tuberculosis, were strongly considered. The “R” marker indicates the right side of the patient. The presence of these localized, dense infiltrates in a young patient with prolonged symptoms is a key finding that guided further diagnostic workup.
nvestigations and Management Plan
Initial Investigations:
- Blood cultures showed no growth.
- Abdominal ultrasound and urinalysis were unremarkable, showing no pathology.
- Ophthalmology consultation revealed normal visual fields.
- Blood samples were planned for complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and anti-HIV antibodies.
Current Treatment Regimen (Day 7):
- Teicoplanin intravenously (7th day) with proper doses
- Ceftriaxone intravenously (7th day) with proper doses
- Pantoprazole orally/intravenously with proper doses
- Isoniazid orally (2nd day) with proper doses
- Rifampicin orally (2nd day) with proper doses
- Pyrazinamide orally (2nd day) with proper doses
- Ethambutol orally (2nd day) with proper doses
Please consult your national guidelines for appropriate drug types and dosages, or seek advice from a licensed physician in the relevant department.
Further Diagnostic and Treatment Plan:
- Collection of gastric lavage fluid for Acid-Fast Bacilli (AFB) PCR and culture for three consecutive days.
- Sputum AFB smear and culture were performed, with results showing AFB (++). This finding was crucial in confirming the diagnosis of tuberculosis.
- Teicoplanin and Ceftriaxone were planned to be continued for a total of 10 days.
Discussion
This case highlights the importance of considering atypical presentations and alternative diagnoses when initial treatments fail. The persistent right upper lobe infiltrates on the chest X-ray, coupled with an inadequate response to standard antibiotics for bacterial pneumonia, raised a high index of suspicion for tuberculosis. The subsequent positive AFB smear in the sputum confirmed the diagnosis, allowing for targeted anti-tuberculosis therapy. Early initiation of appropriate anti-tuberculosis medication is critical for effective treatment and preventing further transmission. The patient’s history of a vancomycin reaction also underscores the need for careful medication selection and monitoring.
Disclaimer
This content is intended for educational and informational purposes only and should not be considered medical advice. It is not a substitute for professional medical diagnosis, treatment, or care. Always seek the advice of a qualified healthcare provider for any questions regarding your medical condition or treatment.

