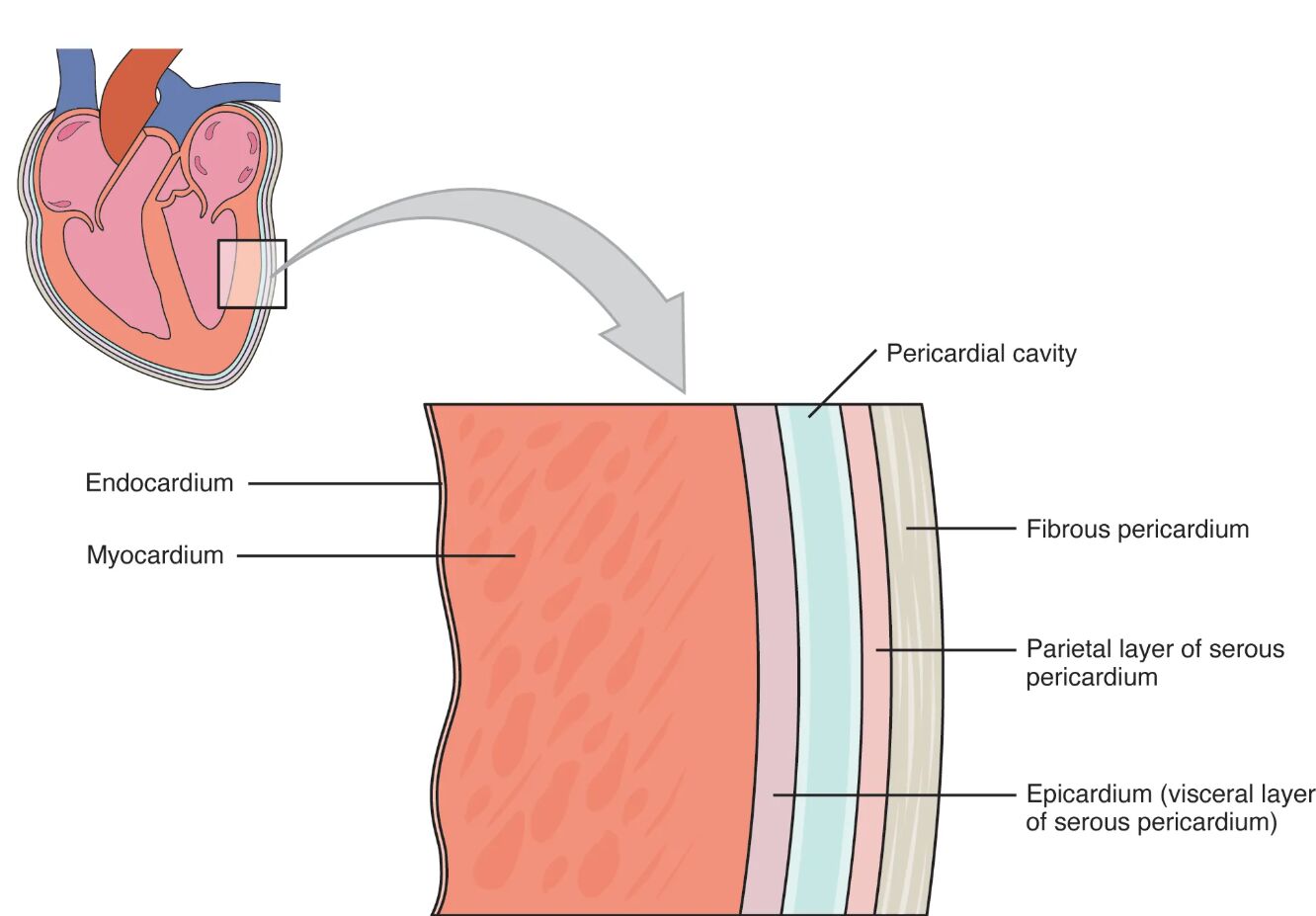
The heart is enveloped by a protective pericardial membrane, a critical structure that supports its function and movement within the chest. This diagram illustrates the three layers of the pericardium and the pericardial cavity, alongside the three layers of the heart wall, with a shared epicardium linking these structures. Delving into this image provides a deeper understanding of the heart’s anatomy and the protective mechanisms that ensure its efficient operation.
Labelled Parts Explanation
- Endocardium The endocardium is the innermost layer of the heart wall, lining the chambers and valves with a smooth endothelial surface. It plays a key role in reducing friction as blood flows through the heart.
- Myocardium The myocardium is the thick, muscular middle layer of the heart wall responsible for contraction and pumping blood. Its robust structure enables the heart to generate the force needed for circulation.
- Pericardial cavity The pericardial cavity is a thin space between the visceral and parietal layers of the serous pericardium, filled with pericardial fluid. This fluid reduces friction during heartbeats, allowing smooth movement.
- Fibrous pericardium The fibrous pericardium is the tough outer layer that anchors the heart to surrounding structures and provides physical protection. It also prevents overexpansion of the heart during increased pressure.
- Parietal layer of serous pericardium The parietal layer of serous pericardium is the outer layer of the serous membrane, lining the fibrous pericardium. It works with the visceral layer to contain the pericardial fluid.
- Epicardium (visceral layer of serous pericardium) The epicardium, or visceral layer of serous pericardium, is the outermost layer of the heart wall and adheres to the myocardium. It serves as a protective barrier and is continuous with the parietal layer at the base of the heart.
Anatomical Overview of the Pericardium and Heart Wall
The pericardium and heart wall are integral to cardiovascular function. This diagram showcases the layered structure that safeguards the heart while enabling its rhythmic contractions.
- The pericardial cavity contains pericardial fluid, which lubricates the heart and reduces friction during movement.
- The fibrous pericardium offers structural support, anchoring the heart within the mediastinum.
- The endocardium and myocardium form the heart’s internal framework, with the myocardium providing the contractile force.
- The epicardium links the heart wall to the parietal layer of serous pericardium, ensuring a seamless protective envelope.
This layered design protects the heart from external trauma and maintains its position for optimal function.
Structure and Function of the Pericardial Layers
The pericardial layers work together to protect and support the heart. Each layer has a specific role in maintaining cardiac efficiency.
- The fibrous pericardium acts as a sturdy outer shell, preventing overstretching and providing attachment points.
- The parietal layer of serous pericardium collaborates with the epicardium to enclose the pericardial cavity.
- The pericardial fluid within the pericardial cavity minimizes friction, allowing the heart to beat without resistance.
- Inflammation of these layers, known as pericarditis, can impair this protective function.
This synergy ensures the heart operates smoothly within a stable environment.
Layers of the Heart Wall Explained
The heart wall comprises three distinct layers, each contributing to its pumping mechanism. This structure is essential for sustaining blood circulation.
- The endocardium provides a smooth lining that prevents blood clot formation and supports valve function.
- The myocardium contains cardiac muscle fibers that contract to propel blood through the circulatory system.
- The epicardium serves as a protective outer layer, also housing coronary blood vessels that supply the heart.
- The thickness of the myocardium varies, with the left ventricle requiring more muscle due to higher pressure demands.
These layers work in unison to maintain the heart’s structural integrity and contractile strength.
Physiological Role of the Pericardial Cavity
The pericardial cavity plays a crucial role in cardiac physiology. Its fluid content is vital for heart movement and protection.
- The pericardial cavity holds approximately 15-50 mL of pericardial fluid, acting as a lubricant.
- This fluid reduces wear on the epicardium and parietal layer of serous pericardium during each heartbeat.
- Excess fluid accumulation can lead to cardiac tamponade, compressing the heart and hindering function.
- The cavity’s small volume ensures the heart remains in place while allowing flexibility.
This balance is essential for uninterrupted cardiac performance.
Clinical Relevance of Pericardial and Heart Wall Layers
Understanding the anatomy of the pericardium and heart wall has significant clinical implications. These structures can be affected by various conditions that impact heart health.
- The fibrous pericardium can become rigid in constrictive pericarditis, limiting heart expansion.
- Damage to the endocardium may lead to endocarditis, an infection that affects the inner heart lining.
- The myocardium’s health is critical, as myocardial infarction (heart attack) results from its oxygen deprivation.
- The epicardium may show inflammation in pericarditis, often causing chest pain.
Monitoring these layers through imaging or physical exams aids in diagnosing and treating cardiac issues.
Conclusion
The diagram of the pericardial membranes and layers of the heart wall offers a detailed look at the protective and functional anatomy surrounding the heart. By exploring the roles of the endocardium, myocardium, epicardium, and pericardial layers, one gains insight into how the heart is shielded and supported during its relentless task of pumping blood. This knowledge serves as a valuable resource for understanding cardiovascular anatomy and addressing related health concerns, encouraging further study of the heart’s intricate design and its clinical significance.

