Introduction:
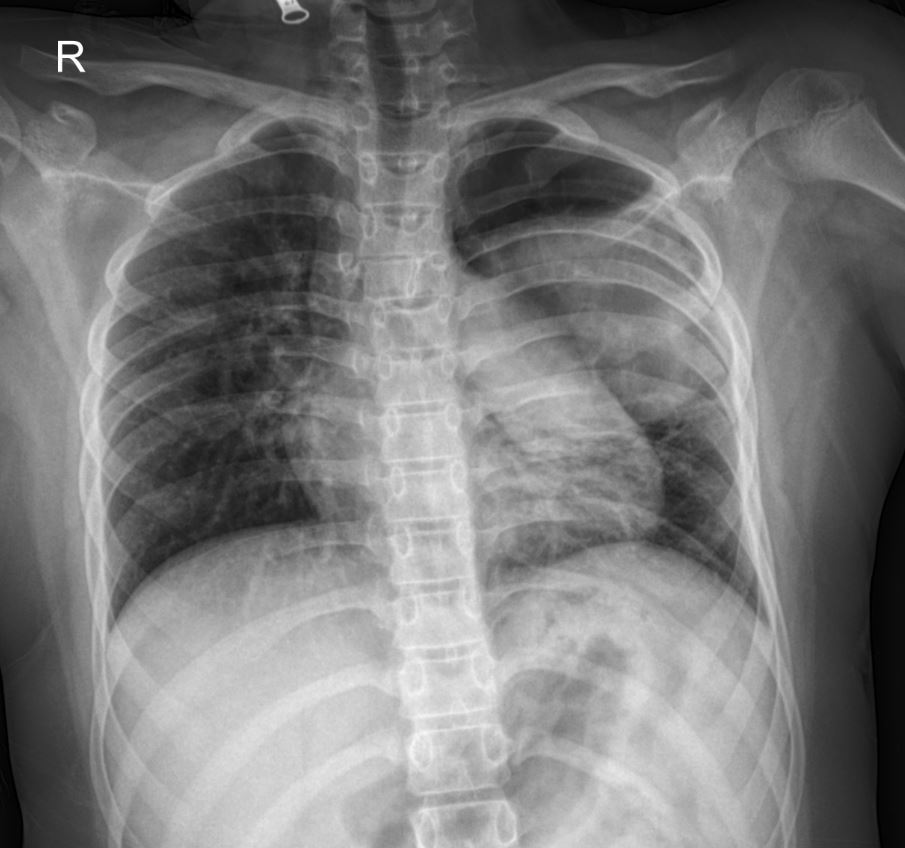
This case study presents a compelling diagnostic challenge in a 12-year-old male patient presenting with acute respiratory symptoms and a significant finding on chest radiography. The presented X-ray image (PA view) reveals a striking abnormality in the left lung, which, when correlated with the patient’s history and further imaging, highlights the complexities of pediatric pulmonary pathology.
Patient Presentation:
A 12-year-old, 6-month-old male patient presented to the emergency department with a 4-day history of cough and hemoptysis that began the previous night. Physical examination revealed decreased breath sounds and rales in the left lung. Laboratory findings included a CRP of 120 mg/L, WBC of 8.1 x 10^9/L, and Platelets of 340 x 10^9/L.
Radiological Findings (Initial PA Chest X-ray):
The initial posteroanterior (PA) chest X-ray image provided offers a critical first look. Observe the left hemithorax, particularly the upper lobe. A large, ill-defined lucency with surrounding consolidation is evident. This appearance strongly suggests a cavitary lesion, an important finding that immediately raises the differential diagnoses of lung abscess, tuberculosis, or even less common etiologies in this age group. The significant size of the lesion is also notable, prompting urgent further investigation.
Past Medical History:
The patient’s past medical history is highly relevant. At 5 years of age, he was hospitalized for 38 days due to pneumonia and effusion in the right lung, requiring two thoracostomy tube insertions. He had no subsequent complaints until the current presentation. This history of severe previous lung infection suggests a potential predisposition to pulmonary complications or the possibility of a chronic underlying condition.
Further Investigations and Management:
Given the X-ray findings and clinical presentation, a thoracic CT scan was performed. The CT report described: “A cavitary lesion approximately 8×9 cm in size, containing air foci and a soft tissue component, was noted in the upper lobe of the left lung. Clinical correlation with the patient’s findings is recommended.”
The patient was consulted with a pediatric infectious disease specialist and admitted to the ward with a provisional diagnosis of lung abscess vs. tuberculosis.
On day 1 of hospitalization, the patient’s general condition was moderate, and vital signs were stable. Respiratory examination continued to show decreased breath sounds and rales in the left lung, with no signs of respiratory distress.
Treatment Initiated:
Initial treatment commenced with broad-spectrum antibiotics:
- Vancomycin: with proper doses
- Meropenem: with proper doses
Please note: Drug types and dosages should be determined based on your country’s relevant pharmaceutical guidelines or by consulting a licensed physician in the relevant department.
Additional Diagnostic Tests:
- ARB test (acid-fast bacilli) on gastric aspirate
- PPD (purified protein derivative) test
- Hydatid cyst serology
- Consultations with relevant departments
Thoracic Ultrasound Findings:
Thoracic ultrasound revealed no pleural effusion in the supradiaphragmatic areas bilaterally. In the middle segment of the left upper lung lobe, lung parenchyma movement indicating aeration was not observed in M-mode, suggesting atelectasis or pneumonia in a patient with a history of thoracic surgery. Clinical and laboratory correlation, with further investigation if necessary, was recommended.
CT Scan Findings (Detailed):
- Trachea and mediastinum were midline.
- Heart size was normal; no pericardial effusion.
- Major vascular structures (aorta) were normal.
- No pathologically enlarged lymph nodes in the mediastinum.
- Lung Parenchyma: “A cavitary lesion approximately 8×9 cm in size, containing air foci and a soft tissue component, was noted in the upper lobe of the left lung. Clinical correlation with the patient’s findings is recommended.”
- No bilateral pleural effusion.
- No acute pathology in incidental bone structures.
Discussion:
This case highlights the importance of integrating clinical presentation, past medical history, and multi-modal imaging in diagnosing complex lung pathologies in children. The large cavitary lesion seen on the X-ray and confirmed by CT demands a thorough workup to differentiate between infectious etiologies like lung abscess (bacterial) and tuberculosis, especially given the patient’s previous severe pneumonia. The history of right-sided disease at 5 years of age and current left-sided involvement prompts consideration of underlying conditions that may predispose to recurrent or persistent lung pathology.
Conclusion:
The chest X-ray in this case serves as a crucial initial imaging modality, clearly demonstrating a significant cavitary lesion in the left upper lobe. This finding, combined with the patient’s symptoms and history, guides the subsequent diagnostic and therapeutic steps. Further investigations are underway to pinpoint the exact etiology of this complex lung lesion.
This content is for educational purposes only and should not be used as a basis for diagnosis or treatment. Always consult with a qualified healthcare professional for medical advice.

