The regulation of blood calcium levels is a finely tuned process involving parathyroid hormone (PTH) and calcitonin, which work together to maintain homeostasis. This article explores a diagram illustrating how PTH increases calcium when levels drop and how calcitonin from the thyroid gland lowers them when they rise, ensuring a balanced physiological state.
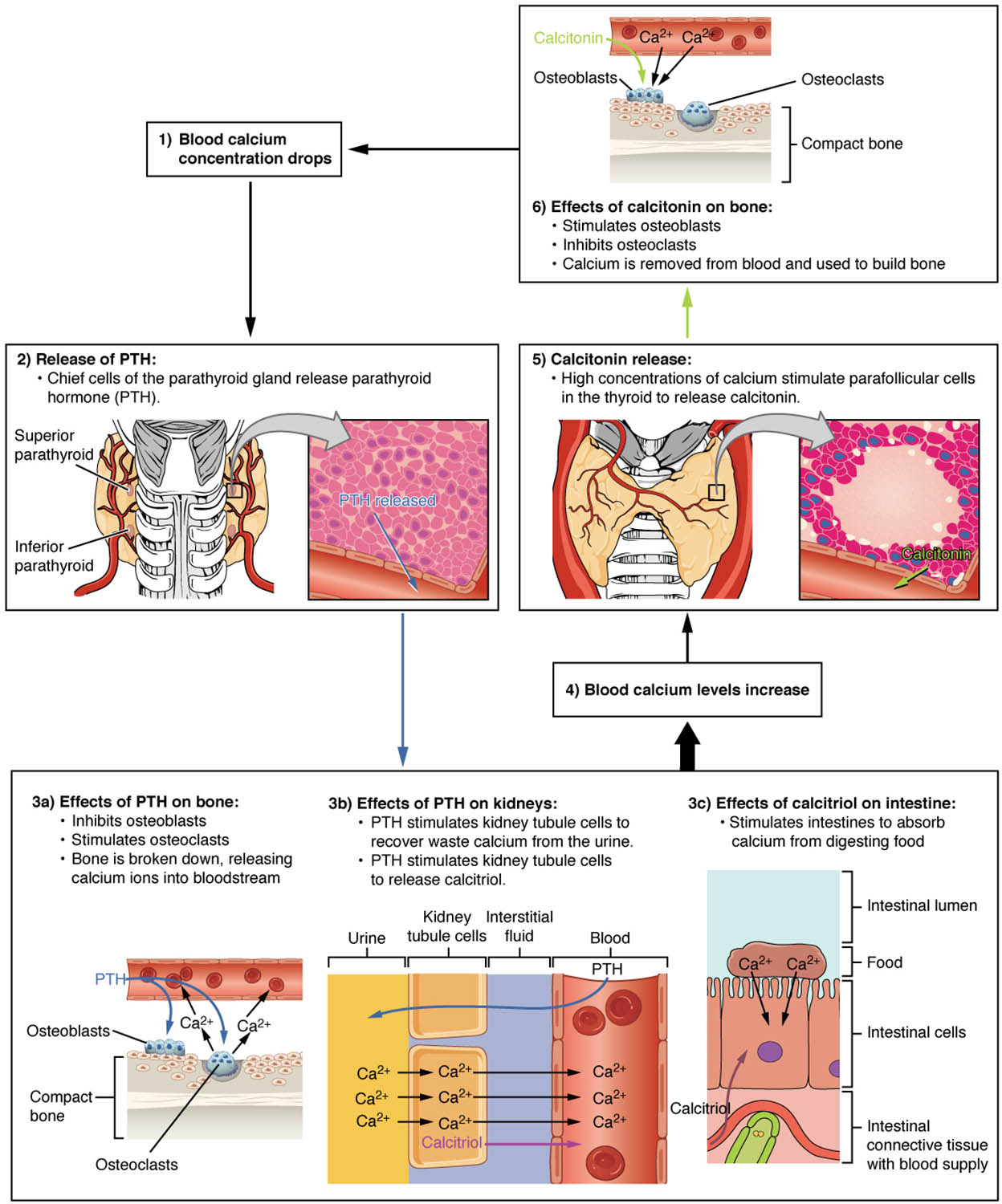
Low blood calcium Low blood calcium levels signal the parathyroid glands to release PTH, initiating a corrective response. This condition prompts the body to restore calcium to normal levels to support critical functions.
Parathyroid glands release PTH The parathyroid glands release PTH when blood calcium is low, stimulating bone resorption and kidney reabsorption. This hormone acts swiftly to elevate calcium concentrations in the bloodstream.
PTH acts on bones PTH acts on bones by promoting the breakdown of bone matrix to release calcium into the blood. This process involves osteoclast activation to maintain skeletal and systemic calcium balance.
PTH acts on kidneys PTH acts on kidneys to increase calcium reabsorption and reduce phosphate levels, enhancing blood calcium retention. This action ensures efficient use of filtered calcium during low levels.
PTH acts on intestines (via vitamin D) PTH acts on intestines by stimulating the conversion of vitamin D to its active form, boosting calcium absorption. This indirect effect amplifies dietary calcium uptake to support blood levels.
High blood calcium High blood calcium levels trigger the thyroid gland to release calcitonin, initiating a reduction process. This response prevents hypercalcemia and its associated complications.
Thyroid gland releases calcitonin The thyroid gland releases calcitonin when blood calcium is elevated, inhibiting bone resorption. This hormone works to lower calcium levels by promoting its deposition into bones.
Calcitonin acts on bones Calcitonin acts on bones by inhibiting osteoclast activity, reducing calcium release into the blood. This action helps store excess calcium in the skeletal matrix.
Calcitonin acts on kidneys Calcitonin acts on kidneys by increasing calcium excretion, helping to reduce blood levels. This process complements bone storage to maintain homeostasis.
Normal blood calcium Normal blood calcium reflects a balanced state where PTH and calcitonin activity stabilizes levels. This equilibrium supports essential physiological processes like nerve signaling and muscle contraction.
Overview of Calcium Homeostasis Mechanisms
The interplay between PTH and calcitonin maintains blood calcium within a narrow range. This dynamic regulation is critical for overall health and function.
- Low blood calcium triggers PTH release from the parathyroid glands.
- PTH enhances calcium release from bones, kidneys, and intestines.
- High blood calcium prompts calcitonin secretion from the thyroid gland.
- Calcitonin reduces calcium by acting on bones and kidneys.
- Normal blood calcium indicates effective hormonal balance.
Role of Parathyroid Hormone in Calcium Regulation
PTH is a key player in correcting low calcium levels. Its multifaceted actions ensure rapid restoration of homeostasis.
- The parathyroid glands sense low blood calcium and release PTH.
- PTH stimulates osteoclasts in bones to release stored calcium.
- Kidney reabsorption under PTH influence conserves calcium.
- The activation of vitamin D by PTH boosts intestinal absorption.
- This coordinated response prevents hypocalcemia-related issues.
Function of Calcitonin in Calcium Control
Calcitonin counters high calcium levels with targeted actions. Its role complements PTH to maintain balance.
- The thyroid gland releases calcitonin in response to elevated calcium.
- Calcitonin inhibits bone resorption, storing excess calcium.
- Kidney excretion of calcium is enhanced by calcitonin.
- This mechanism prevents hypercalcemia and supports bone health.
- The process ensures calcium levels remain within normal limits.
Physiological and Clinical Significance
The PTH-calcitonin axis is vital for calcium homeostasis and overall physiology. Understanding this system aids in clinical practice.
- Normal blood calcium supports nerve conduction and muscle function.
- Imbalances can lead to hypocalcemia, causing tetany or seizures.
- Hypercalcemia from excessive PTH may result in kidney stones.
- Blood tests measure calcium, PTH, and calcitonin levels for diagnosis.
- Treatments adjust hormone activity to restore balance.
The precise regulation of blood calcium through the actions of parathyroid hormone and calcitonin highlights the body’s ability to maintain homeostasis. This dynamic interplay between the parathyroid and thyroid glands ensures calcium levels support vital functions while preventing disease, offering a foundation for exploring endocrine health and related interventions.

