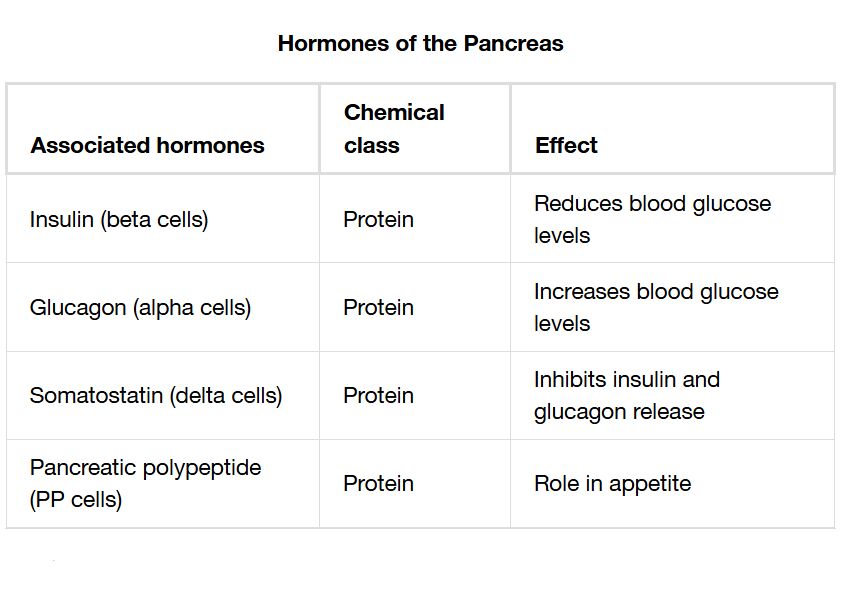
The pancreas, a dual-function organ, serves as both an exocrine and endocrine gland, playing a pivotal role in digestion and blood sugar regulation. This article delves into a detailed chart of the hormones produced by the pancreas, exploring their release mechanisms and physiological effects, offering a thorough understanding of their impact on metabolic health.
Pancreas The pancreas is located in the abdomen, behind the stomach, functioning as both an exocrine and endocrine organ. Its endocrine role involves hormone secretion into the bloodstream to regulate glucose levels.
Islets of Langerhans The islets of Langerhans are clusters of endocrine cells within the pancreas that produce hormones. These specialized cells are critical for maintaining blood sugar homeostasis.
Alpha cells Alpha cells within the islets secrete glucagon to raise blood glucose levels during fasting or hypoglycemia. They respond to low glucose concentrations to prevent energy deficits.
Beta cells Beta cells produce insulin, which lowers blood glucose by promoting its uptake into cells. They are activated when glucose levels rise, such as after a meal.
Delta cells Delta cells release somatostatin, which inhibits the secretion of other pancreatic hormones and digestive enzymes. This hormone helps regulate the overall endocrine activity of the pancreas.
Glucagon Glucagon increases blood glucose by stimulating glycogen breakdown and gluconeogenesis in the liver. It is released when blood sugar levels drop, ensuring energy availability.
Insulin Insulin facilitates glucose uptake by cells, reducing blood sugar levels and promoting energy storage. Its secretion is triggered by elevated glucose, such as postprandial states.
Somatostatin Somatostatin modulates the release of glucagon and insulin, fine-tuning glucose regulation. It also inhibits digestive processes, coordinating pancreatic function.
Effects Effects of pancreatic hormones include blood sugar regulation, energy storage, and digestive control. These outcomes maintain metabolic stability and support overall health.
Anatomical Structure of the Pancreas
The pancreas combines exocrine and endocrine functions within its structure. This dual role enhances its ability to regulate digestion and metabolism.
- The pancreas is situated behind the stomach, extending horizontally across the abdomen.
- The islets of Langerhans house endocrine cells, distinct from exocrine acinar cells.
- Alpha, beta, and delta cells within the islets perform specialized hormonal roles.
- Its location near major blood vessels ensures efficient hormone distribution.
- This anatomy supports both local and systemic physiological effects.
Hormone Production in the Islets of Langerhans
The islets of Langerhans contain distinct cell types that produce specific hormones. Their coordinated activity maintains glucose homeostasis.
- Alpha cells secrete glucagon to counteract low blood sugar.
- Beta cells release insulin to manage high glucose levels.
- Delta cells produce somatostatin to regulate hormone release.
- These cells respond to blood glucose changes via feedback mechanisms.
- The islets’ cellular diversity ensures balanced metabolic control.
Physiological Roles of Pancreatic Hormones
Pancreatic hormones play a critical role in glucose metabolism and energy balance. Their actions are essential for daily physiological function.
- Glucagon stimulates liver glycogenolysis and gluconeogenesis during fasting.
- Insulin promotes glucose uptake into muscles and fat cells for storage.
- Somatostatin inhibits excessive glucagon or insulin release.
- These hormones work in concert to prevent hyperglycemia or hypoglycemia.
- Their effects extend to lipid and protein metabolism as well.
Clinical Relevance and Associated Disorders
Understanding pancreatic hormones aids in diagnosing and managing metabolic diseases. Imbalances can lead to significant health challenges.
- Insufficient insulin production causes diabetes mellitus, leading to hyperglycemia.
- Excess glucagon can contribute to diabetic ketoacidosis in uncontrolled diabetes.
- Overactive delta cells may disrupt hormone balance, affecting digestion.
- Blood tests measure insulin, glucagon, and glucose levels for diagnosis.
- Treatments include insulin therapy or dietary management to restore balance.
The pancreas, through its islets of Langerhans, orchestrates a sophisticated system of hormone release to regulate blood sugar and support metabolic health. The interplay of glucagon, insulin, and somatostatin ensures energy availability and storage, while disorders like diabetes mellitus highlight the importance of this regulation. This knowledge provides a foundation for exploring pancreatic function and effective clinical interventions.

