The heart’s rhythmic beating is a marvel of biological engineering, ensuring continuous blood circulation through a well-coordinated process known as the cardiac cycle. This diagram illustrates the phases of the cardiac cycle—atrial systole, ventricular systole, atrial diastole, and ventricular diastole—while correlating these events with an electrocardiogram (ECG) for a clearer understanding of electrical and mechanical activity. Exploring this cycle provides valuable insights into how the heart maintains life-sustaining circulation, making it an essential topic for those interested in cardiovascular health.
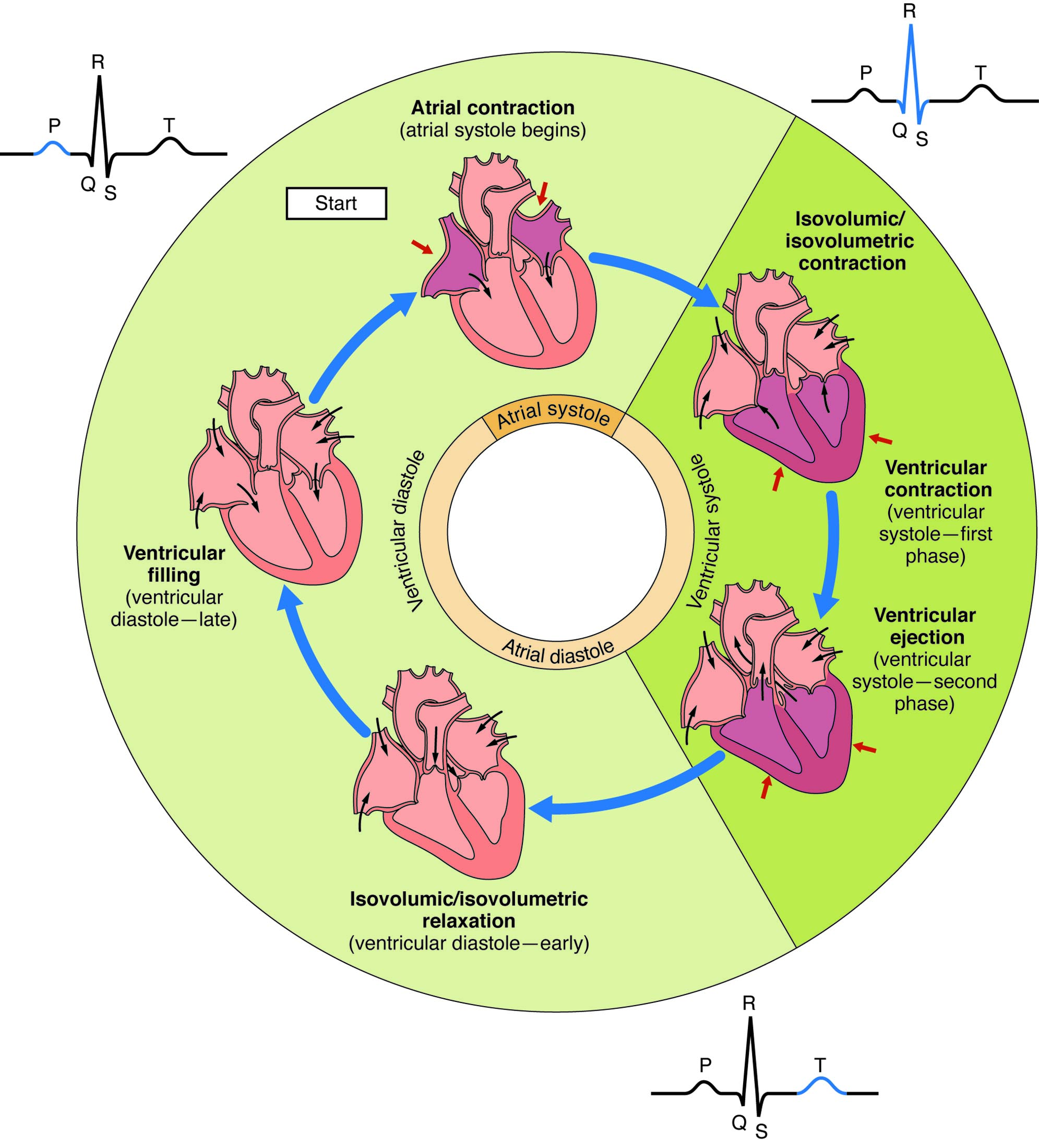
Atrial systole Atrial systole is the phase where the atria contract, pushing blood into the ventricles just before ventricular contraction begins. This process is triggered by the P wave on the ECG, ensuring the ventricles are fully primed for the next phase.
Ventricular systole Ventricular systole involves the contraction of the ventricles, ejecting blood into the pulmonary artery and aorta, marked by the QRS complex on the ECG. This phase generates the pressure needed to circulate blood throughout the body and lungs.
Atrial diastole Atrial diastole is the relaxation phase of the atria, allowing them to fill with blood returning from the veins, corresponding to the T wave and early P wave preparation on the ECG. This passive filling ensures the atria are ready for the next contraction.
Ventricular diastole Ventricular diastole is the relaxation and filling phase of the ventricles, where they receive blood from the atria and prepare for the next cycle, aligned with the T wave on the ECG. This period includes isovolumetric relaxation and rapid filling, critical for maintaining cardiac output.
Phases of the Cardiac Cycle
The cardiac cycle consists of distinct phases that ensure efficient heart function. This diagram outlines their sequence and timing.
- Atrial systole contributes about 20-30% of ventricular filling, enhancing stroke volume.
- Ventricular systole generates the “lub” sound (S1) as the atrioventricular valves close.
- Atrial diastole allows passive blood flow, supported by venous return pressure.
- Ventricular diastole produces the “dub” sound (S2) with semilunar valve closure.
- The cycle repeats approximately 60-100 times per minute at rest.
Correlation with the Electrocardiogram (ECG)
The ECG provides a window into the electrical events of the cardiac cycle. This diagram links these signals to mechanical actions.
- The P wave signals atrial systole, initiating atrial depolarization.
- The QRS complex marks ventricular systole, reflecting ventricular depolarization.
- The T wave corresponds to ventricular diastole, indicating ventricular repolarization.
- The PR interval shows the delay at the AV node, coordinating atrial and ventricular activity.
- These correlations help diagnose rhythm abnormalities or conduction issues.
Mechanical Events in Atrial Systole
Atrial systole actively contributes to ventricular filling. Its timing is crucial for efficient pumping.
- This phase begins with atrial depolarization, seen as the P wave on the ECG.
- The atria contract, forcing blood through the open mitral and tricuspid valves.
- Atrial kick boosts end-diastolic volume, especially in conditions like atrial fibrillation.
- The process lasts about 0.1 seconds, ensuring minimal overlap with ventricular action.
- Increased atrial pressure aids filling in cases of reduced ventricular compliance.
Dynamics of Ventricular Systole
Ventricular systole drives blood circulation through powerful contractions. This phase is the heart’s main pumping effort.
- It starts with the QRS complex, triggering rapid ventricular contraction.
- The atrioventricular valves close, marking the beginning of isovolumetric contraction.
- Blood is ejected as semilunar valves open, propelled into the aorta and pulmonary artery.
- The phase ends with the T wave, as ventricular pressure drops below arterial pressure.
- Stroke volume depends on this phase’s efficiency, influenced by preload and contractility.
Relaxation Phases: Atrial and Ventricular Diastole
Diastole allows the heart to rest and refill, preparing for the next cycle. This diagram highlights its dual components.
- Atrial diastole occurs as the atria relax, filling with blood from the superior and inferior vena cava.
- Ventricular diastole follows, with isovolumetric relaxation as all valves are closed briefly.
- Rapid filling then occurs as the AV valves open, driven by atrial pressure.
- The T wave signifies repolarization, enabling ventricular relaxation.
- This phase occupies about two-thirds of the cardiac cycle at rest.
Physiological Regulation of the Cardiac Cycle
The cardiac cycle is finely tuned by neural and hormonal controls. These mechanisms adapt to bodily demands.
- The autonomic nervous system modulates heart rate, speeding it up with sympathetic input.
- Parasympathetic stimulation via the vagus nerve slows the cycle during rest.
- Baroreceptors adjust cycle length based on blood pressure changes.
- Thyroid hormones like T3 and T4 enhance metabolic rate, influencing cardiac output.
- These regulators ensure the cycle meets varying physiological needs.
Clinical Significance of the Cardiac Cycle
Understanding the cardiac cycle aids in diagnosing heart conditions. This diagram supports clinical evaluations.
- Irregular atrial systole may indicate atrial fibrillation, reducing atrial contribution.
- Prolonged ventricular systole can suggest aortic stenosis, increasing afterload.
- Atrial diastole abnormalities might reflect mitral valve issues, impairing filling.
- Ventricular diastole dysfunction is common in heart failure, reducing compliance.
- Echocardiography and ECG analysis monitor these phases for treatment planning.
Impact of Age and Lifestyle
Age and lifestyle influence the cardiac cycle’s efficiency. This diagram prompts consideration of these factors.
- Aging stiffens ventricles, prolonging ventricular diastole and reducing filling.
- Regular exercise enhances atrial systole strength, improving cardiac reserve.
- Poor diet can lead to atherosclerosis, affecting ventricular systole output.
- Smoking increases sympathetic tone, shortening diastolic phases.
- Hydration and stress management support optimal cycle performance.
Advances in Cardiac Cycle Research
Ongoing studies refine our understanding of this process. This diagram inspires innovative approaches.
- High-resolution ECG mapping tracks micro-variations in the cardiac cycle.
- 3D echocardiography visualizes atrial systole and ventricular diastole dynamics.
- Wearable devices monitor cycle phases in real-time for health tracking.
- Gene therapy explores enhancing myocardial contractility in systole.
- These advancements improve diagnosis and management of cardiac conditions.
In conclusion, this diagram of the cardiac cycle offers a detailed overview of the heart’s rhythmic phases—atrial systole, ventricular systole, atrial diastole, and ventricular diastole—correlated with ECG patterns for a comprehensive understanding. This cycle ensures the continuous flow of blood, supporting life through coordinated electrical and mechanical events. By exploring its anatomy, regulation, and clinical relevance, we can better appreciate its role in health and leverage advancements to enhance cardiovascular care and treatment outcomes.

