This article provides a comprehensive overview of mitral regurgitation (MR), a common valvular heart disease, as clearly depicted in the provided diagram. We will explore the critical function of the mitral valve, detail how its malfunction leads to inefficient blood flow, and discuss the subsequent physiological consequences on the heart’s pumping efficiency and overall cardiovascular health. This detailed explanation aims to inform both medical professionals and individuals seeking to understand this significant cardiac pathology.
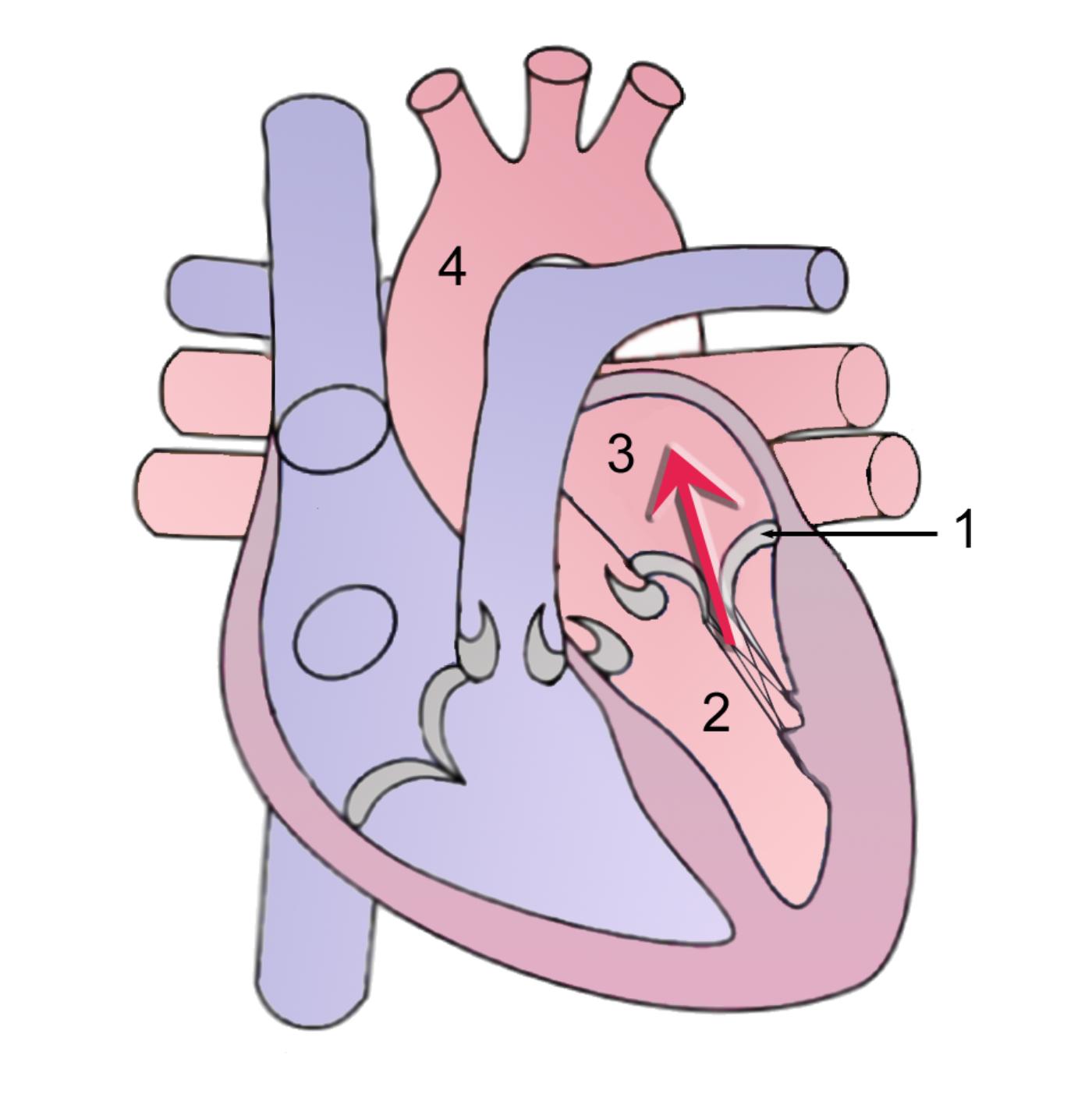
1: Mitral Valve: This label indicates the mitral valve, located between the left atrium and the left ventricle. In this diagram, it is depicted as not closing completely during ventricular contraction, which is the hallmark of mitral regurgitation.
2: Left Ventricle: This is the heart’s strongest pumping chamber, responsible for ejecting oxygenated blood into the aorta for systemic circulation. In mitral regurgitation, it has to pump extra volume due to backward blood flow from the mitral valve.
3: Left Atrium: This chamber receives oxygenated blood from the lungs via the pulmonary veins and normally passes it into the left ventricle. In mitral regurgitation, it receives backward blood flow from the left ventricle, leading to enlargement and increased pressure.
4: Aorta: The body’s largest artery, originating from the left ventricle, responsible for distributing oxygenated blood to the entire body. While directly receiving blood from the left ventricle, in MR, the effective forward flow into the aorta is reduced due to the backward leak through the mitral valve.
Mitral regurgitation (MR) is a condition where the mitral valve, located between the left atrium and the left ventricle, fails to close properly during ventricular contraction (systole). This improper closure allows blood to leak backward from the left ventricle into the left atrium, rather than flowing forward into the aorta. The diagram provides a clear illustration of this phenomenon, showing the mitral valve (1) with an abnormal opening during systole, allowing blood (indicated by the red arrow) to flow back into the left atrium (3). This inefficient blood movement places an extra burden on the heart, leading to a cascade of physiological changes that can compromise cardiac function and overall health.
The presence of mitral regurgitation means that the left ventricle must pump a larger volume of blood with each beat to ensure adequate forward flow to the body, as a portion of the ejected blood is lost to the left atrium. This chronic volume overload leads to compensatory changes in the heart, including enlargement of the left atrium and left ventricle. Over time, these adaptations can become detrimental, potentially leading to symptoms of heart failure and other severe complications.
Understanding the mechanisms and causes of mitral regurgitation is crucial for timely diagnosis and effective management. The condition can be acute or chronic, with different etiologies and clinical presentations.
- Leaky Valve: The mitral valve does not close completely during ventricular systole.
- Backward Blood Flow: Blood regurgitates from the left ventricle into the left atrium.
- Volume Overload: The left atrium and left ventricle handle an increased volume of blood.
These factors contribute to the progressive nature and potential severity of mitral regurgitation.
The Pathophysiology of Mitral Regurgitation
The pathophysiology of mitral regurgitation revolves around the failure of the mitral valve apparatus to maintain its integrity during left ventricular systole. The mitral valve apparatus consists of the valve leaflets, chordae tendineae (fibrous cords that anchor the leaflets), papillary muscles (muscle projections in the ventricle that support the chordae), and the mitral annulus (the fibrous ring around the valve opening). Any pathology affecting one or more of these components can lead to MR. When the valve leaflets do not coapt (meet) properly, a gap remains, through which blood flows backward into the left atrium (3) during ventricular contraction.
This regurgitant volume causes a chronic volume overload in both the left atrium and the left ventricle (2). The left atrium dilates to accommodate the extra blood volume, leading to increased pressure within the atrium and subsequently in the pulmonary veins and capillaries, which can cause pulmonary congestion and shortness of breath. The left ventricle also dilates and hypertrophies (thickens) in an attempt to maintain forward cardiac output, as it must pump both the blood intended for the aorta and the regurgitant volume. Over time, this chronic strain can lead to progressive left ventricular dysfunction, impaired contractility, and ultimately, heart failure. The severity of MR depends on the size of the regurgitant orifice, the pressure difference between the left ventricle and left atrium during systole, and the duration of regurgitation.
Causes and Clinical Manifestations
Mitral regurgitation can be classified as primary (organic), due to intrinsic valve leaflet or subvalvular apparatus abnormalities, or secondary (functional), due to ventricular remodeling that prevents leaflet coaptation without primary leaflet disease. Common causes of primary MR include:
- Mitral valve prolapse: The most common cause, where the valve leaflets bulge into the left atrium during systole.
- Rheumatic heart disease: Inflammation that can cause scarring and deformity of the valve leaflets.
- Endocarditis: Infection of the valve leaflets, leading to destruction.
- Myocardial infarction: Can cause rupture of papillary muscles or chordae tendineae.
- Congenital abnormalities: Present from birth.
Secondary MR often occurs in conditions like dilated cardiomyopathy or ischemic heart disease, where the left ventricle enlarges, pulling the papillary muscles and chordae tendineae apart, preventing the leaflets from closing effectively.
Symptoms of MR often develop gradually over many years, particularly in chronic cases. Patients may remain asymptomatic for a long time, but as the condition progresses, they can experience fatigue, shortness of breath (dyspnea), especially during exertion or when lying flat (orthopnea), and palpitations. In severe cases, MR can lead to the development of heart failure, atrial fibrillation (an irregular heart rhythm), or pulmonary hypertension. Acute MR, such as from papillary muscle rupture after a heart attack, is a medical emergency with sudden onset of severe dyspnea and cardiogenic shock. Physical examination often reveals a characteristic holosystolic murmur heard best at the apex of the heart, radiating to the axilla.
Diagnosis and Management Strategies
Diagnosing mitral regurgitation involves a comprehensive approach, starting with a detailed medical history and physical examination. Auscultation of the heart typically reveals the characteristic heart murmur. An electrocardiogram (ECG) may show signs of left atrial enlargement or left ventricular hypertrophy. A chest X-ray can indicate an enlarged heart silhouette and pulmonary congestion. However, the definitive diagnostic tool is an echocardiogram. This non-invasive imaging technique provides detailed real-time images of the heart’s structure, allowing visualization of the mitral valve leaflets, assessment of the severity of regurgitation, quantification of the regurgitant volume, and evaluation of left ventricular and left atrial size and function. Transesophageal echocardiography may be used for a more detailed assessment, particularly if valve repair is being considered.
Management of MR depends on its severity, the presence of symptoms, and the impact on left ventricular function. For mild to moderate, asymptomatic MR with preserved left ventricular function, careful monitoring with regular echocardiograms is usually sufficient. Medications such as diuretics can help manage symptoms of fluid overload, and vasodilators (e.g., ACE inhibitors) may be used in certain cases to reduce afterload and improve forward flow. However, for severe, symptomatic MR, or even asymptomatic severe MR with early signs of left ventricular dysfunction or dilation, surgical intervention is often recommended. This involves either mitral valve repair (mitral valvuloplasty), which is generally preferred to preserve the patient’s native valve, or mitral valve replacement with a mechanical or bioprosthetic valve. The timing of surgery is crucial to prevent irreversible damage to the left ventricle and ensure optimal long-term outcomes.

