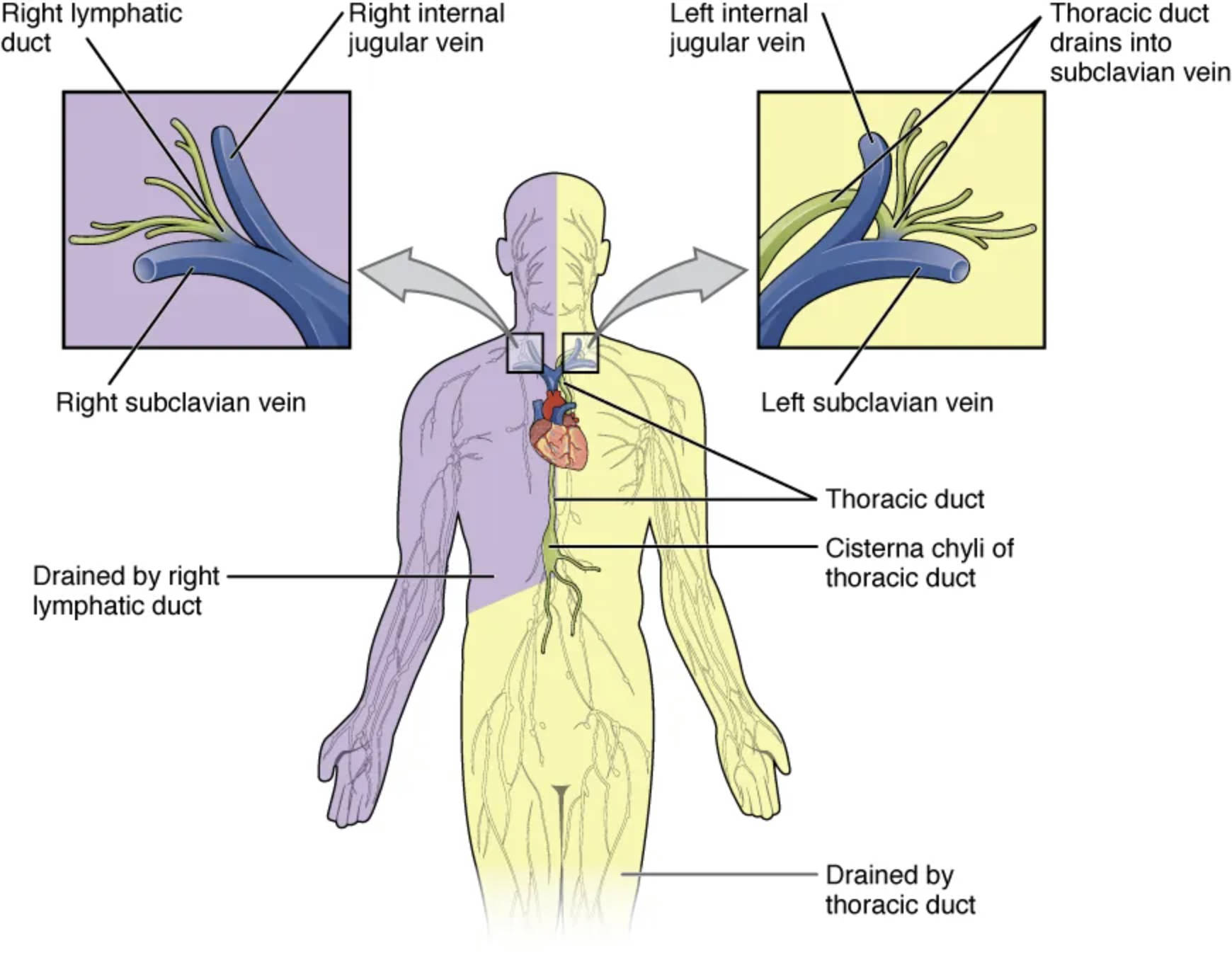
The lymphatic system’s major trunks and ducts are essential for returning lymph to the bloodstream, playing a key role in fluid balance and immune defense. This diagram illustrates the primary pathways, including the thoracic duct and right lymphatic duct, highlighting their distinct drainage regions and connections to the venous system.
Key Labeled Components in the Lymphatic System Diagram
Right lymphatic duct The right lymphatic duct collects lymph from the right upper body, including the right arm, chest, and head, draining it into the bloodstream. This relatively short duct ensures efficient fluid return from a smaller portion of the body compared to the thoracic duct.
Right subclavian vein The right subclavian vein receives lymph from the right lymphatic duct, serving as the entry point into the venous system. Located near the collarbone, it facilitates the mixing of lymph with blood for recirculation.
Right internal jugular vein The right internal jugular vein, paired with the subclavian vein, accepts lymph from the right lymphatic duct, draining the head and neck region. This vein plays a crucial role in returning lymph from the cranial tissues to the heart.
Drained by right lymphatic duct The area drained by the right lymphatic duct encompasses the right side of the head, neck, and upper limb, covering approximately one-fifth of the body’s lymph. This region’s lymph is filtered through nodes before reaching this duct for venous return.
Left subclavian vein The left subclavian vein collects lymph from the thoracic duct, serving as the primary entry point for lymph from the lower body and left upper body. Its position near the heart ensures efficient reintegration into the circulatory system.
Left internal jugular vein The left internal jugular vein, alongside the left subclavian vein, receives lymph from the thoracic duct, draining the left side of the head and neck. This vessel supports the return of lymph from the cranial region to the bloodstream.
Thoracic duct The thoracic duct is the body’s largest lymphatic vessel, draining lymph from the lower limbs, abdomen, left thorax, and left arm, covering about four-fifths of the body. It originates from the cisterna chyli and empties into the left subclavian vein near the junction with the jugular vein.
Cisterna chyli of thoracic duct The cisterna chyli is a dilated sac at the lower end of the thoracic duct, collecting lymph from the abdominal region and lower limbs. This reservoir ensures a steady flow of lymph upward through the thoracic duct for eventual venous return.
Drained by thoracic duct The area drained by the thoracic duct includes the majority of the body, such as the left side of the head, neck, chest, abdomen, and both lower limbs. This extensive drainage underscores its critical role in maintaining fluid homeostasis.
Thoracic duct drains into subclavian vein The thoracic duct drains into the left subclavian vein, marking the point where lymph re-enters the bloodstream after filtration. This junction is vital for preventing fluid buildup and supporting circulatory function.
Role of Major Lymphatic Ducts in Fluid Balance
The thoracic duct and right lymphatic duct are central to maintaining bodily fluids. Their distinct drainage areas ensure comprehensive lymph collection.
- Thoracic Duct Dominance: Draining over 75% of the body’s lymph, the thoracic duct handles a larger volume, originating from the cisterna chyli to manage lower body fluids.
- Right Lymphatic Duct Efficiency: This duct manages the right upper quadrant, quickly returning lymph to the venous system via the right subclavian vein.
- Venous Integration: Both ducts empty into subclavian veins, preventing edema by returning excess interstitial fluid to circulation.
The lymphatic system relies on these ducts’ coordinated action, driven by muscle movement and respiratory pressure. This process supports immune function by transporting antigens to lymph nodes.
Anatomical Pathways and Structural Features
The pathways of these ducts reveal their complexity. Each duct’s connection to the venous system is precisely engineered.
- Thoracic Duct Length: Spanning from the abdomen to the left clavicle, this duct includes valves to ensure upward flow against gravity.
- Cisterna Chyli Function: Acting as a lymph reservoir, it collects fluid from intestinal and lumbar trunks, stabilizing flow into the thoracic duct.
- Right Lymphatic Duct Compactness: Its shorter length and direct drainage into the right venous angle optimize upper body lymph return.
Valves within the ducts prevent backflow, a feature critical for efficient lymph movement. The thoracic duct’s larger capacity reflects its broader drainage territory.
Integration with Immune and Circulatory Systems
These ducts link the lymphatic system with immune and circulatory networks. This integration enhances overall health.
The thoracic duct transports chylomicrons—lipid particles—from the gut, bypassing initial blood filtration for metabolic efficiency. Lymph carried by both ducts contains immune cells like lymphocytes, which are filtered in nodes before venous return.
- Immune Transport: Antigens in lymph trigger responses in lymph nodes, with ducts delivering processed lymph to the bloodstream.
- Fluid Regulation: Returning 2-4 liters of lymph daily, these ducts prevent hypotension and tissue swelling.
- Circulatory Support: The subclavian vein junctions ensure lymph re-enters near the heart, aiding cardiac output.
This synergy highlights the ducts’ role in homeostasis and defense.
In conclusion, the major trunks and ducts of the lymphatic system, including the thoracic duct and right lymphatic duct, are vital for fluid balance and immune support. Their anatomical design and integration with the circulatory system underscore their importance in maintaining health and resilience.

