Discover the vital process of internal respiration, where oxygen is delivered from the bloodstream to body cells, and carbon dioxide, a metabolic waste product, is collected for transport back to the lungs. This article elucidates the crucial diffusion across tissue capillaries and the roles of plasma and red blood cells in sustaining cellular life.
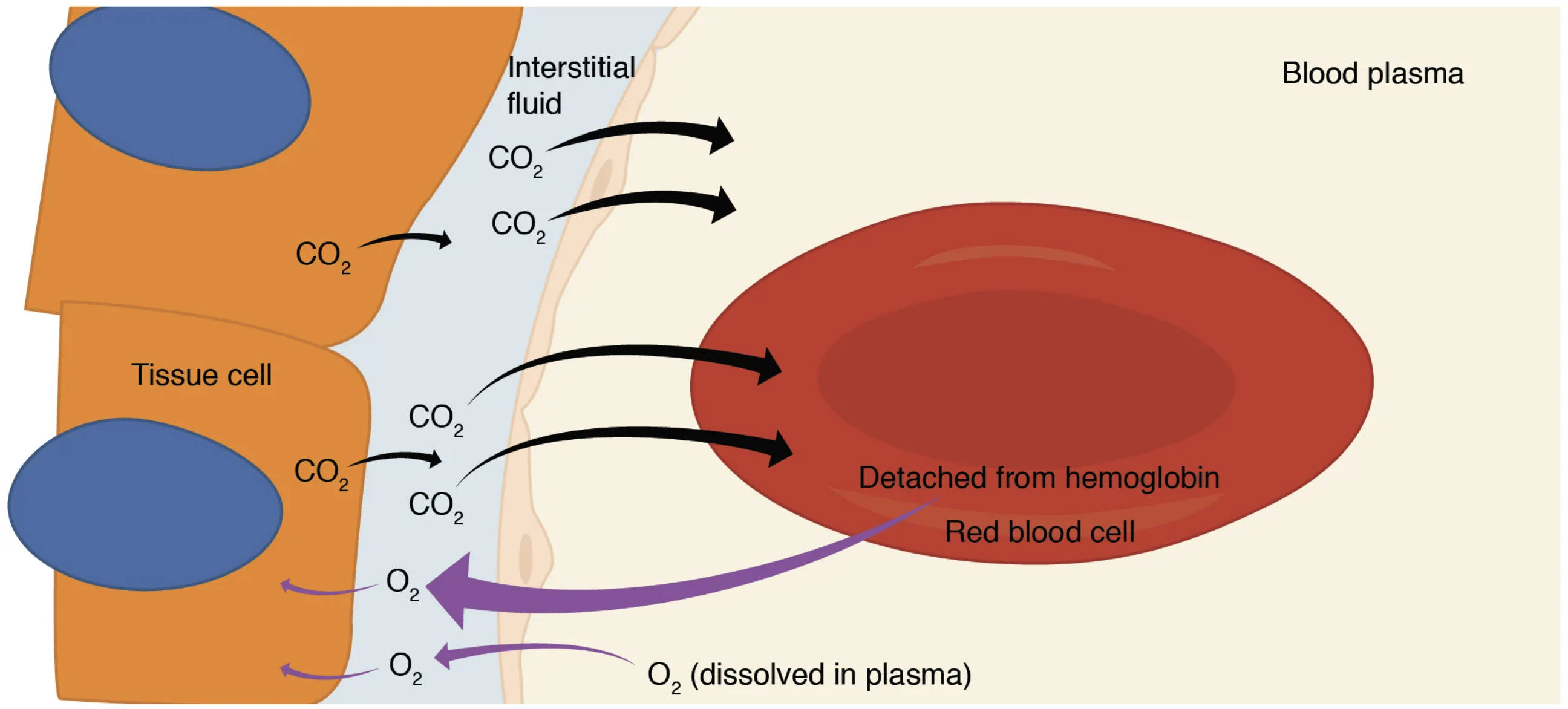
Interstitial fluid: This is the fluid that surrounds the tissue cells, acting as a medium for the exchange of substances between the blood capillaries and the cells. Oxygen diffuses from the capillaries into this fluid, and then into the cells, while carbon dioxide moves in the opposite direction.
CO2 (carbon dioxide): This is a metabolic waste product produced by tissue cells during cellular respiration. Its diffusion out of the cells and into the blood is a critical aspect of internal respiration, preventing its accumulation which can lead to acidosis.
Tissue cell: These are the individual cells throughout the body that perform various metabolic functions, continuously consuming oxygen and producing carbon dioxide. The exchange of these gases at the tissue cell level is what defines internal respiration.
Blood plasma: This is the liquid component of blood, accounting for about 55% of total blood volume. It serves as a transport medium for dissolved gases, nutrients, waste products, and hormones, playing a role in carrying oxygen and carbon dioxide during internal respiration.
Detached from hemoglobin: This refers to oxygen molecules that have been released from their binding sites on hemoglobin within the red blood cell. This detachment is essential for oxygen to diffuse out of the red blood cell and into the surrounding tissues.
Red blood cell: These cells, also known as erythrocytes, are the primary carriers of oxygen in the blood due to their high concentration of hemoglobin. During internal respiration, red blood cells release oxygen to the tissues and take up carbon dioxide to transport it back to the lungs.
O2 (dissolved in plasma): A small fraction of oxygen is transported dissolved directly in the blood plasma. This dissolved oxygen contributes to the partial pressure gradient that drives oxygen from the capillaries into the interstitial fluid and then into the tissue cells.
The Body’s Silent Exchange: Understanding Internal Respiration
Internal respiration is a fundamental physiological process that ensures every cell in the body receives the oxygen it needs to function and that metabolic waste product, carbon dioxide, is effectively removed. Unlike external respiration, which occurs in the lungs, internal respiration takes place at the cellular level, specifically between the systemic capillaries and the body’s tissue cells. This continuous exchange of gases is vital for sustaining cellular metabolism and maintaining overall bodily homeostasis.
The efficiency of internal respiration hinges on the precise interplay of partial pressure gradients, facilitating the diffusion of oxygen from the blood into the cells and carbon dioxide from the cells into the blood. This intricate process involves the blood plasma, red blood cells, and the interstitial fluid that bathes the tissue cells, acting as an intermediary for gas transfer.
Key elements of internal respiration include:
- Oxygen delivery from blood to tissue cells.
- Carbon dioxide collection from tissue cells into the blood.
- Diffusion driven by partial pressure gradients.
This continuous exchange is what keeps our cells energized and functioning optimally.
Oxygen Delivery: Fueling Cellular Activity
The process of internal respiration begins with the arrival of oxygen-rich blood at the systemic capillaries, having been oxygenated in the lungs during external respiration. The primary goal at this stage is to deliver oxygen to the metabolically active tissue cells, where it is consumed in cellular respiration to produce energy.
Oxygen’s Path to the Tissue Cells
The blood flowing through the capillaries has a higher partial pressure of oxygen (PO2) than the surrounding interstitial fluid and the tissue cells, which are constantly consuming oxygen. This partial pressure gradient is the driving force behind oxygen’s movement. First, oxygen, both dissolved in the blood plasma and bound to hemoglobin within the red blood cells, begins to diffuse out of the capillaries. The oxygen bound to hemoglobin within the red blood cells detaches from hemoglobin (HbO2 → O2 + HHb), allowing it to then diffuse out of the red blood cells.
Once released from the red blood cells, oxygen diffuses through the capillary wall and into the interstitial fluid. From the interstitial fluid, it then crosses the cell membrane to enter the individual tissue cell. This continuous supply of oxygen is critical for aerobic cellular respiration, the process by which cells generate adenosine triphosphate (ATP) for their various functions. Factors such as lower pH (more acidic environment due to CO2 and lactic acid), higher temperature, and increased levels of 2,3-bisphosphoglycerate (BPG) in active tissues all contribute to a decreased affinity of hemoglobin for oxygen, promoting oxygen release where it is most needed (the Bohr effect).
Carbon Dioxide Pickup: Removing Metabolic Waste
As tissue cells consume oxygen and produce energy, they simultaneously generate carbon dioxide (CO2) as a waste product of cellular metabolism. The efficient removal of this CO2 is just as crucial as oxygen delivery, as its accumulation can lead to detrimental changes in blood pH (acidosis).
Carbon Dioxide’s Journey from Cells to Blood
The tissue cell has a significantly higher partial pressure of carbon dioxide (PCO2) compared to the interstitial fluid and the blood in the systemic capillaries. This creates a strong gradient that drives the CO2 out of the cells. The carbon dioxide first diffuses from the tissue cells into the interstitial fluid. From the interstitial fluid, it then readily diffuses across the capillary wall and into the bloodstream.
Once in the blood, carbon dioxide is transported back to the lungs via three main mechanisms:
- Dissolved in Plasma: A small percentage of CO2 (about 7-10%) remains dissolved directly in the blood plasma.
- Bound to Hemoglobin: Approximately 20-30% of CO2 binds to the amino groups of hemoglobin, forming carbaminohemoglobin (CO2 + Hb ⇌ HbCO2). This binding is facilitated by the release of oxygen from hemoglobin (the Haldane effect), which increases hemoglobin’s affinity for CO2.
- As Bicarbonate Ions: The most significant portion of CO2 (about 70%) is transported as bicarbonate ions (HCO3-). Inside the red blood cells, CO2 combines with water (H2O) to form carbonic acid (H2CO3), catalyzed by the enzyme carbonic anhydrase. Carbonic acid then dissociates into H+ and HCO3-. The bicarbonate ions move into the plasma in exchange for chloride ions (chloride shift), while the H+ ions bind to deoxyhemoglobin, buffering the blood pH. This efficient transport mechanism ensures CO2 is carried away from the tissues without causing severe pH imbalances.
Conclusion
Internal respiration is a ceaseless, vital process that underscores the efficiency of our circulatory and respiratory systems. It is the silent, yet profound, exchange of gases at the cellular level, ensuring that tissue cells receive the life-sustaining oxygen they require while simultaneously ridding the body of metabolic waste in the form of carbon dioxide. Understanding this intricate interplay of diffusion, partial pressures, and biochemical reactions is fundamental to appreciating the body’s remarkable capacity for maintaining homeostasis and is essential knowledge in the realm of medical science.

