The kidneys play a pivotal role in regulating blood pressure and blood volume through a sophisticated interplay of hormones and physiological responses. This diagram highlights the short-term and long-term mechanisms, including the renin-angiotensin-aldosterone system and erythropoietin production, which work together to restore homeostasis and maintain cardiovascular stability.
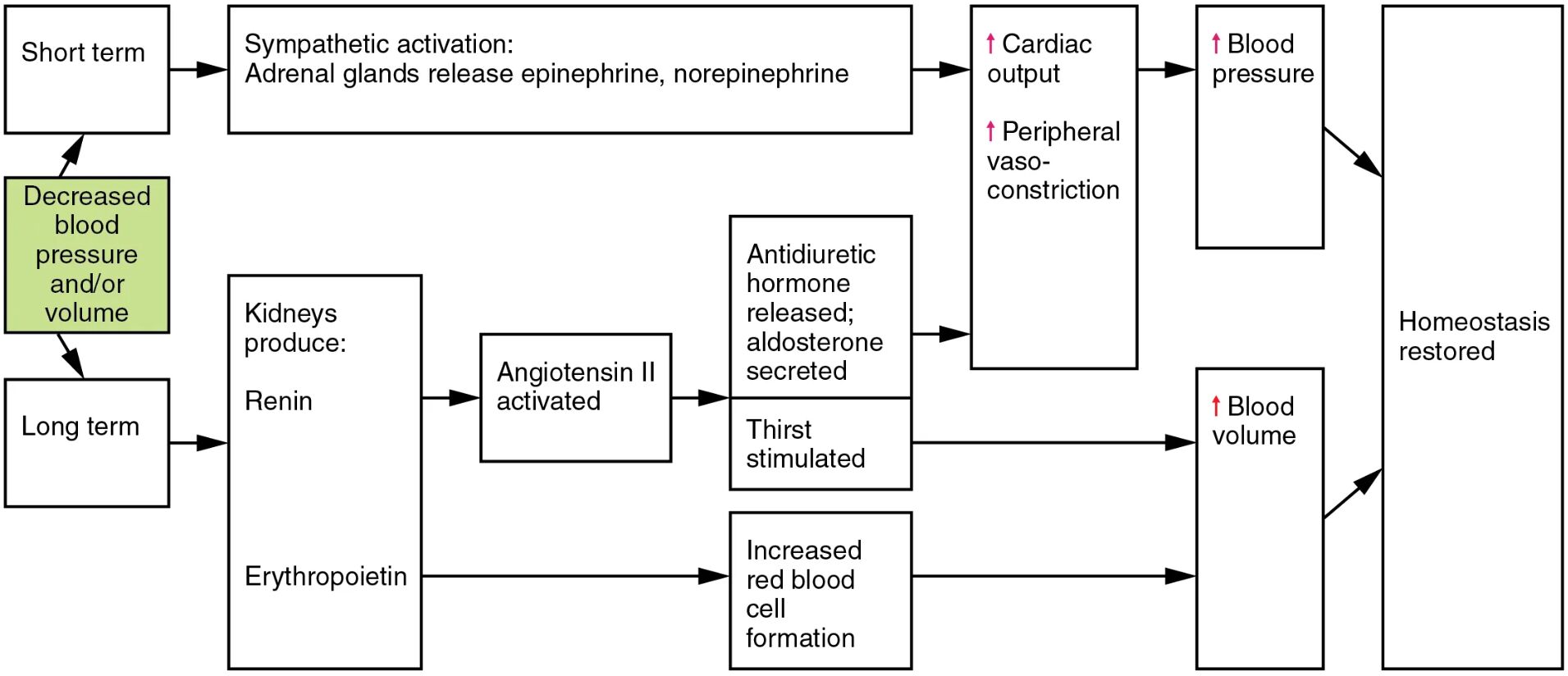
Short term This phase involves rapid responses to changes in blood pressure or volume. It activates the sympathetic nervous system to provide immediate adjustments.
Decreased blood pressure and/or volume A drop in these parameters signals the body to initiate compensatory mechanisms. This triggers the release of hormones to restore normal levels.
Kidneys produce: Renin The kidneys release renin in response to low blood pressure or volume, initiating the renin-angiotensin-aldosterone cascade. This enzyme converts angiotensinogen to angiotensin I, setting the stage for further regulation.
Angiotensin II activated Angiotensin II is a potent vasoconstrictor formed from angiotensin I by ACE. It stimulates thirst, increases blood pressure, and triggers the release of aldosterone and antidiuretic hormone.
Sympathetic activation: Adrenal glands release epinephrine, norepinephrine This activation enhances cardiac output and causes peripheral vasoconstriction. Epinephrine and norepinephrine from the adrenal glands provide a rapid boost to circulation.
Antidiuretic hormone released; aldosterone secreted Antidiuretic hormone reduces water loss by promoting reabsorption in the kidneys. Aldosterone enhances sodium retention, increasing blood volume and pressure.
Thirst stimulated Angiotensin II drives the sensation of thirst to encourage fluid intake. This helps elevate blood volume to counteract the initial decrease.
Cardiac output Increased heart rate and contractility boost cardiac output to raise blood pressure. This response supports short-term circulatory needs.
Peripheral vasoconstriction Narrowing of blood vessels increases peripheral resistance, elevating blood pressure. This action complements cardiac output to stabilize circulation.
Blood pressure The combined effects lead to a rise in blood pressure, addressing the initial decrease. This restores adequate perfusion to vital organs.
Long term This phase focuses on sustained regulation of blood volume and pressure. It involves additional hormonal adjustments for long-lasting balance.
Erythropoietin Produced by the kidneys, erythropoietin stimulates red blood cell formation. This increases oxygen-carrying capacity and indirectly supports blood volume.
Increased red blood cell formation More red blood cells enhance blood viscosity and volume over time. This contributes to sustained improvements in blood pressure and oxygen delivery.
Blood volume Elevated blood volume supports long-term pressure stability. It ensures the circulatory system can meet ongoing metabolic demands.
Homeostasis restored Through these mechanisms, the body returns to a balanced state, maintaining optimal blood pressure and volume. This restoration supports overall health and resilience.
The Role of the Renin-Angiotensin-Aldosterone System
Renin production marks the beginning of a critical pathway in blood pressure regulation. This enzyme, released by the juxtaglomerular cells, responds to decreased renal perfusion.
- Renin cleaves angiotensinogen into angiotensin I, a precursor to more active forms.
- The process accelerates when blood pressure drops, ensuring a rapid hormonal response.
- Angiotensin-converting enzyme (ACE) in the lungs converts angiotensin I to angiotensin II.
- This system is vital during dehydration or hemorrhage, stabilizing circulation.
- Inhibitors of this pathway, like ACE inhibitors, are used to manage hypertension.
Short-Term Responses to Blood Pressure Changes
Sympathetic activation provides an immediate reaction to decreased blood pressure and/or volume. This rapid response engages the adrenal glands and cardiovascular system.
- Epinephrine increases heart rate and contractility, boosting cardiac output.
- Norepinephrine induces peripheral vasoconstriction to raise vascular resistance.
- These hormones act within seconds, offering a quick fix to hypotension.
- The effect is temporary, paving the way for longer-term adjustments.
- Overactivation can lead to stress-related cardiovascular strain.
Long-Term Regulation with Erythropoietin
Erythropoietin offers a sustained approach to maintaining blood volume and pressure. Produced by the kidneys in response to low oxygen levels, it supports red blood cell production.
- Increased red blood cell formation enhances oxygen delivery to tissues.
- This process indirectly boosts blood volume by improving hematocrit levels.
- The effect develops over days to weeks, complementing short-term fixes.
- It is particularly important in chronic conditions like anemia or hypoxia.
- Synthetic erythropoietin is used clinically to treat renal failure patients.
Hormonal Actions of Angiotensin II
Angiotensin II serves as a central player in both short- and long-term regulation. Its activation triggers multiple downstream effects to restore homeostasis.
- It stimulates thirst to increase fluid intake, raising blood volume.
- Aldosterone secretion promotes sodium and water retention in the kidneys.
- Antidiuretic hormone enhances water reabsorption, further elevating volume.
- Vasoconstriction of arterioles increases peripheral resistance.
- These actions collectively stabilize blood pressure over varying timescales.
Achieving Homeostasis Through Integrated Responses
The interplay of short-term and long-term mechanisms ensures homeostasis is restored effectively. This integrated approach addresses both immediate and sustained needs.
- Cardiac output and vasoconstriction provide rapid pressure increases.
- Increased blood volume from hormonal actions supports long-term stability.
- The feedback loop adjusts hormone levels once balance is achieved.
- Dysregulation can lead to conditions like hypertension or edema.
- Understanding these processes aids in developing targeted therapies.
The kidneys’ hormonal control over blood pressure and volume showcases the body’s remarkable adaptability. Through the coordinated efforts of renin, angiotensin II, and erythropoietin, the circulatory system maintains equilibrium, offering insights into both health and potential interventions.

