The body employs intricate mechanisms to counteract a decrease in blood pressure and volume, ensuring survival during conditions like hemorrhage or dehydration. This diagram illustrates the neural and endocrine responses that stimulate cardiovascular adjustments and hormone release, ultimately restoring homeostasis to maintain circulatory stability.
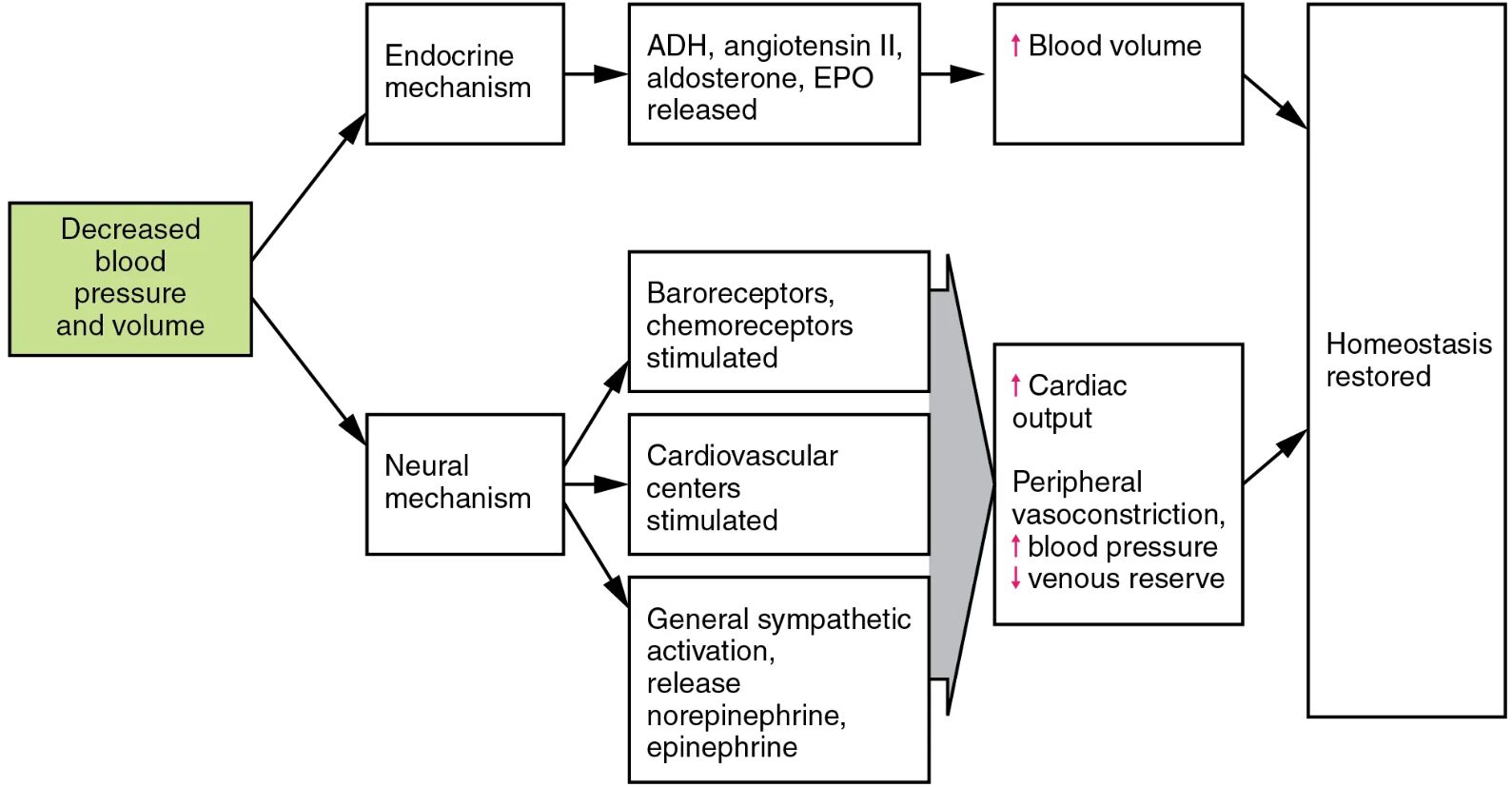
Decreased blood pressure and volume This condition triggers the body’s compensatory responses when blood loss or fluid depletion occurs. It activates both neural and endocrine systems to restore normal levels.
Neural mechanism This involves the rapid activation of the nervous system to address immediate changes. It stimulates cardiovascular centers to enhance circulation.
Endocrine mechanism This pathway releases hormones to regulate blood volume over time. It includes the release of ADH, angiotensin II, aldosterone, and EPO to address the deficit.
Baroreceptors, chemoreceptors stimulated These sensors detect drops in pressure and oxygen levels, respectively. They signal the brain to initiate corrective actions to stabilize the system.
Cardiovascular centers stimulated Located in the medulla, these centers coordinate heart and vessel responses. They increase cardiac output and adjust vascular tone.
General sympathetic activation, release norepinephrine, epinephrine This activation boosts heart rate and constricts blood vessels. Norepinephrine and epinephrine from the adrenal glands enhance this rapid response.
Cardiac output Increased heart rate and contractility raise cardiac output to compensate for lost volume. This helps maintain blood pressure in the short term.
Peripheral vasoconstriction, blood pressure Narrowing of peripheral vessels increases resistance, raising blood pressure. This redirection prioritizes vital organ perfusion.
Venous reserve Constriction of veins mobilizes blood from reservoirs to the central circulation. This increases venous return to support cardiac output.
ADH, angiotensin II, aldosterone, EPO released These hormones work to retain water, constrict vessels, and boost red blood cell production. They collectively increase blood volume over time.
Blood volume Restored volume ensures adequate circulation and oxygen delivery. This gradual increase supports long-term stability.
Homeostasis restored Through these integrated responses, the body returns to a balanced state. This restoration prevents organ damage from prolonged low pressure or volume.
Neural Mechanisms in Acute Response
Neural mechanism provides an immediate reaction to decreased blood pressure and volume. Baroreceptors and chemoreceptors play a key role in this rapid adjustment.
- Baroreceptors in the carotid sinus detect pressure drops and signal the brainstem.
- Chemoreceptors respond to reduced oxygen, prompting ventilatory and circulatory changes.
- Sympathetic activation increases heart rate and contractility via norepinephrine.
- Epinephrine enhances this effect, mobilizing energy stores for a quick response.
- This system is critical during acute blood loss, such as in trauma.
Endocrine Regulation of Blood Volume
Endocrine mechanism addresses the long-term restoration of blood volume. Hormones like ADH and angiotensin II are central to this process.
- ADH promotes water reabsorption in the kidneys to retain fluid.
- Angiotensin II constricts blood vessels and stimulates aldosterone release.
- Aldosterone enhances sodium retention, increasing blood volume indirectly.
- EPO boosts red blood cell production, improving oxygen-carrying capacity.
- These hormones work synergistically to prevent hypovolemic shock.
Role of Cardiovascular Centers
Cardiovascular centers stimulated orchestrate the heart and vessel responses to low pressure. This coordination ensures efficient blood distribution.
- The medulla activates sympathetic nerves to increase cardiac output.
- It also triggers peripheral vasoconstriction to redirect blood to vital organs.
- Venous reserve mobilization enhances venous return to the heart.
- This response is fine-tuned to match the severity of volume loss.
- Overactivation can lead to excessive strain on the cardiovascular system.
Impact of Sympathetic Activation
General sympathetic activation, release norepinephrine, epinephrine provides a rapid boost to circulation. This response is vital during acute volume loss.
- Norepinephrine constricts arterioles, raising blood pressure.
- Epinephrine increases heart rate and dilates coronary arteries.
- Together, they enhance cardiac output and peripheral resistance.
- This activation also mobilizes glucose for energy during stress.
- Prolonged activation may contribute to hypertension if unchecked.
Restoring Homeostasis Through Integrated Efforts
The combined efforts of neural and endocrine systems restore homeostasis after blood volume loss. This integrated approach ensures long-term stability.
- Increased cardiac output and vasoconstriction provide immediate pressure support.
- Rising blood volume from hormonal actions sustains circulation.
- The feedback loop adjusts responses once normal levels are achieved.
- Failure of these mechanisms can lead to hypovolemic shock or organ failure.
- Understanding this process aids in managing conditions like hemorrhage.
The body’s ability to respond to decreased blood pressure and volume through neural and endocrine mechanisms is a testament to its resilience. By leveraging cardiovascular centers stimulated, hormonal releases, and sympathetic activation, the system restores homeostasis, offering valuable insights into circulatory health and emergency care.

