Folliculogenesis is the complex and continuous process by which ovarian follicles develop from primordial structures to mature, ovulatory follicles, and eventually regress or ovulate. This intricate sequence, depicted in the diagram, is fundamental to female reproductive function, fertility, and the cyclical production of hormones. Understanding these stages is crucial for comprehending the menstrual cycle and related reproductive health issues.
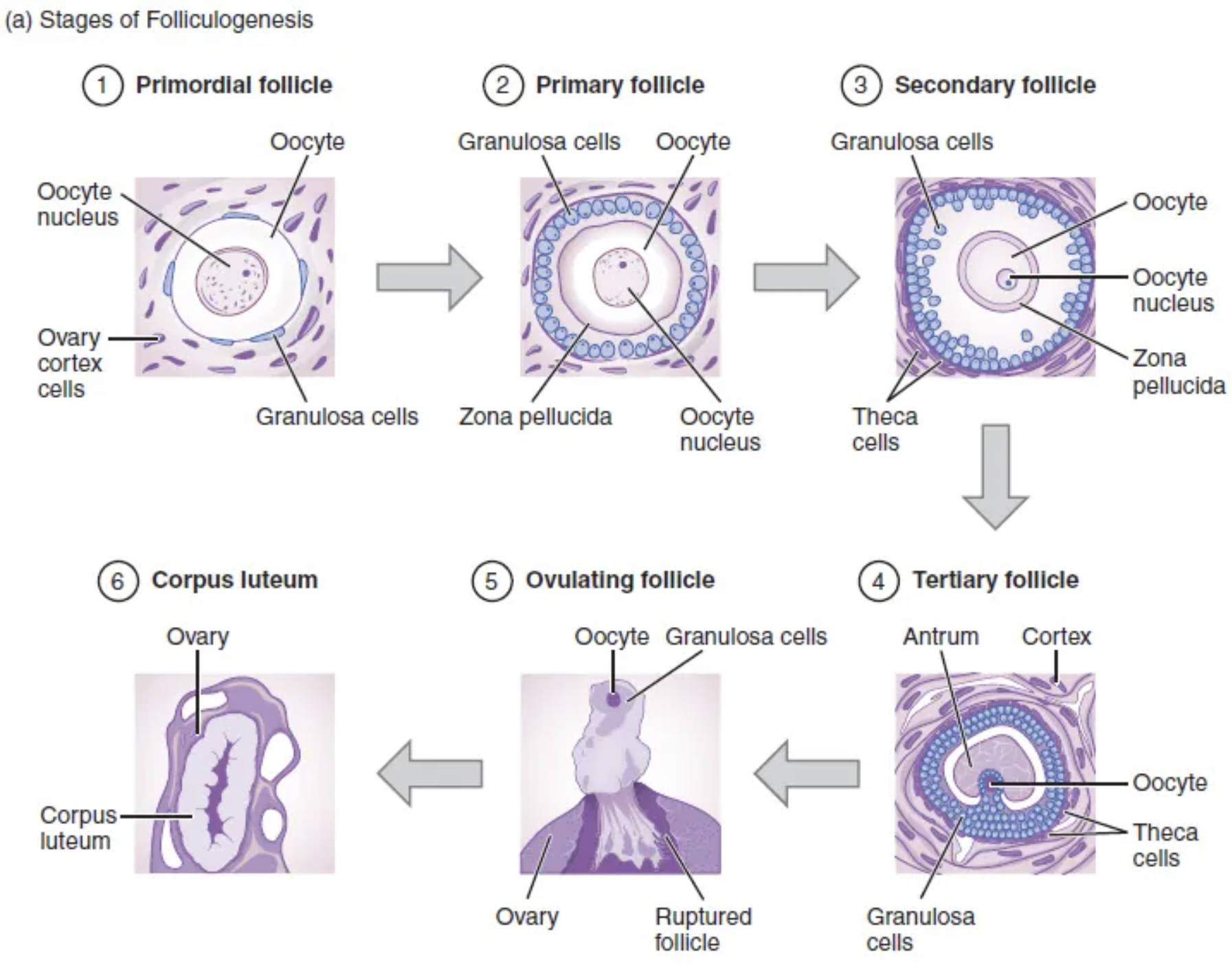
Primordial follicle: A primordial follicle is the earliest stage of ovarian follicle development, present in the fetal ovary and constituting the vast majority of follicles in a woman’s reproductive life. It consists of a primary oocyte arrested in prophase I of meiosis, surrounded by a single layer of flattened granulosa cells.
Oocyte: The oocyte is the immature female gamete, or egg cell, residing within the ovarian follicle. Throughout folliculogenesis, the oocyte grows and undergoes meiotic divisions to eventually become a mature ovum capable of fertilization.
Ovary cortex cells: These cells represent the outer layer of the ovary, where all ovarian follicles are located and develop. The ovarian cortex is rich in connective tissue and houses various stages of developing follicles.
Granulosa cells: Granulosa cells are somatic cells that surround the oocyte within the follicle, playing a critical role in its development and maturation. They produce hormones, primarily estrogen, and provide essential nutrients to the oocyte.
Primary follicle: A primary follicle develops from a primordial follicle, characterized by the enlargement of the oocyte and the transformation of the surrounding granulosa cells from flattened to cuboidal. A thick layer called the zona pellucida also begins to form around the oocyte.
Zona pellucida: The zona pellucida is a transparent, extracellular layer of glycoproteins that surrounds the oocyte, forming a protective barrier. It is crucial for sperm binding and penetration during fertilization, ensuring species-specific interactions.
Oocyte nucleus: The oocyte nucleus contains the genetic material of the female gamete. Its division through meiosis is a central event in oocyte maturation, leading to the reduction of chromosome number.
Secondary follicle: A secondary follicle is distinguished by the proliferation of granulosa cells into multiple layers around the oocyte. The theca cells also begin to differentiate around the outside of the follicle, contributing to hormone production.
Theca cells: Theca cells are stromal cells that differentiate around the developing follicle, forming an outer layer. They work in conjunction with granulosa cells to produce steroid hormones, particularly androgens which are then converted to estrogen by granulosa cells.
Tertiary follicle: A tertiary follicle, also known as an antral follicle, is characterized by the formation of a fluid-filled cavity called the antrum within the granulosa cell layers. This marks a significant stage of growth and hormone production, making the follicle visible by ultrasound.
Antrum: The antrum is a fluid-filled cavity that develops within the granulosa cell mass of a tertiary follicle. The fluid, rich in hormones and growth factors, provides a unique microenvironment for the developing oocyte.
Cortex: The cortex refers to the outer region of the ovary where the follicles are embedded. It is the functional zone of the ovary, housing all the stages of follicle development.
Ovulating follicle: An ovulating follicle, specifically a mature Graafian follicle, is at its largest size and is ready to release the oocyte. Hormonal signals trigger the rupture of this follicle, releasing the secondary oocyte during ovulation.
Ruptured follicle: A ruptured follicle is the remnant of the ovulating follicle after the release of the oocyte. Its structural integrity is lost as the oocyte is expelled from the ovary.
Corpus luteum: The corpus luteum is a temporary endocrine structure that forms from the remnants of the ruptured follicle after ovulation. It primarily produces progesterone, a hormone essential for maintaining the uterine lining and supporting early pregnancy.
The Journey of an Ovarian Follicle
Folliculogenesis is a continuous and complex developmental process within the ovary that underpins female reproductive function. It involves the growth and maturation of ovarian follicles, which are specialized cellular structures that house and nurture developing oocytes. This intricate process spans several distinct stages, from dormant primordial follicles to the release of a mature egg, and its remnants transforming into a temporary endocrine gland. Understanding folliculogenesis is essential for comprehending the menstrual cycle, fertility, and the hormonal regulation of the female body.
The journey of a follicle is a testament to the remarkable precision of biological systems. Only a small fraction of the vast number of primordial follicles present at birth will ever complete the entire developmental pathway to ovulation. Each stage is characterized by specific morphological changes and hormonal interactions, ensuring that the oocyte is properly prepared for potential fertilization. The coordination between the oocyte, granulosa cells, and theca cells is critical for successful maturation.
Key stages of folliculogenesis include:
- Primordial follicle (dormant, single layer of flattened granulosa cells)
- Primary follicle (oocyte enlarges, cuboidal granulosa cells)
- Secondary follicle (multiple layers of granulosa cells, theca cells appear)
- Tertiary/Antral follicle (antrum formation, significant growth)
- Ovulating follicle (Graafian follicle, ready for rupture)
- Corpus luteum (post-ovulation endocrine structure)
Disruptions in folliculogenesis can lead to various reproductive disorders, including infertility and conditions like polycystic ovary syndrome (PCOS), emphasizing the vital importance of this developmental sequence.
Anatomical and Hormonal Dynamics
The process of folliculogenesis is initiated with primordial follicles, which are present in the ovarian cortex from birth. Each primordial follicle consists of a primary oocyte surrounded by a single layer of flattened granulosa cells. Under specific hormonal cues, a cohort of these primordial follicles begins to grow, transitioning into primary follicles. In this stage, the granulosa cells become cuboidal and proliferate, and the zona pellucida starts to form around the oocyte, a critical layer for future sperm interaction. As development continues, the follicle progresses to a secondary stage, characterized by multiple layers of granulosa cells and the differentiation of theca cells in the surrounding stromal tissue. Theca cells are crucial as they work synergistically with granulosa cells to produce estrogens, converting cholesterol into androgens which are then aromatized into estrogen by the granulosa cells.
The transition to a tertiary, or antral, follicle is marked by the formation of a fluid-filled cavity called the antrum within the granulosa cell layers. This antrum grows significantly, making the follicle much larger and increasingly sensitive to pituitary gonadotropins, FSH (Follicle-Stimulating Hormone) and LH (Luteinizing Hormone). Typically, only one tertiary follicle in each cycle becomes dominant and matures into a preovulatory, or Graafian, follicle. This mature follicle is poised for ovulation, a process triggered by a surge in LH. During ovulation, the Graafian follicle ruptures, releasing the secondary oocyte into the fallopian tube. The remaining cells of the ruptured follicle then rapidly transform into the corpus luteum, a temporary endocrine gland. The corpus luteum primarily secretes progesterone, which prepares the uterine lining for potential implantation of a fertilized egg, demonstrating the intricate link between follicle development and the broader menstrual cycle.
In conclusion, folliculogenesis is a fascinating and fundamental process within the female reproductive system, dictating the availability of mature oocytes and the cyclical production of ovarian hormones. From the initial quiescent primordial follicle to the formation of the hormone-producing corpus luteum, each stage is precisely regulated to ensure reproductive success. A comprehensive understanding of these developmental events is essential for appreciating female fertility, addressing reproductive health challenges, and unraveling the complexities of human development.

