Cardiac output is a critical measure of the heart’s efficiency, representing the volume of blood pumped by the heart per minute to meet the body’s demands. This vital physiological parameter depends on two key components: heart rate and stroke volume, each influenced by a variety of factors that ensure adaptability to physical activity, stress, or rest. Understanding these influencing elements provides insight into maintaining cardiovascular health and optimizing bodily functions, making this topic essential for anyone interested in heart physiology.
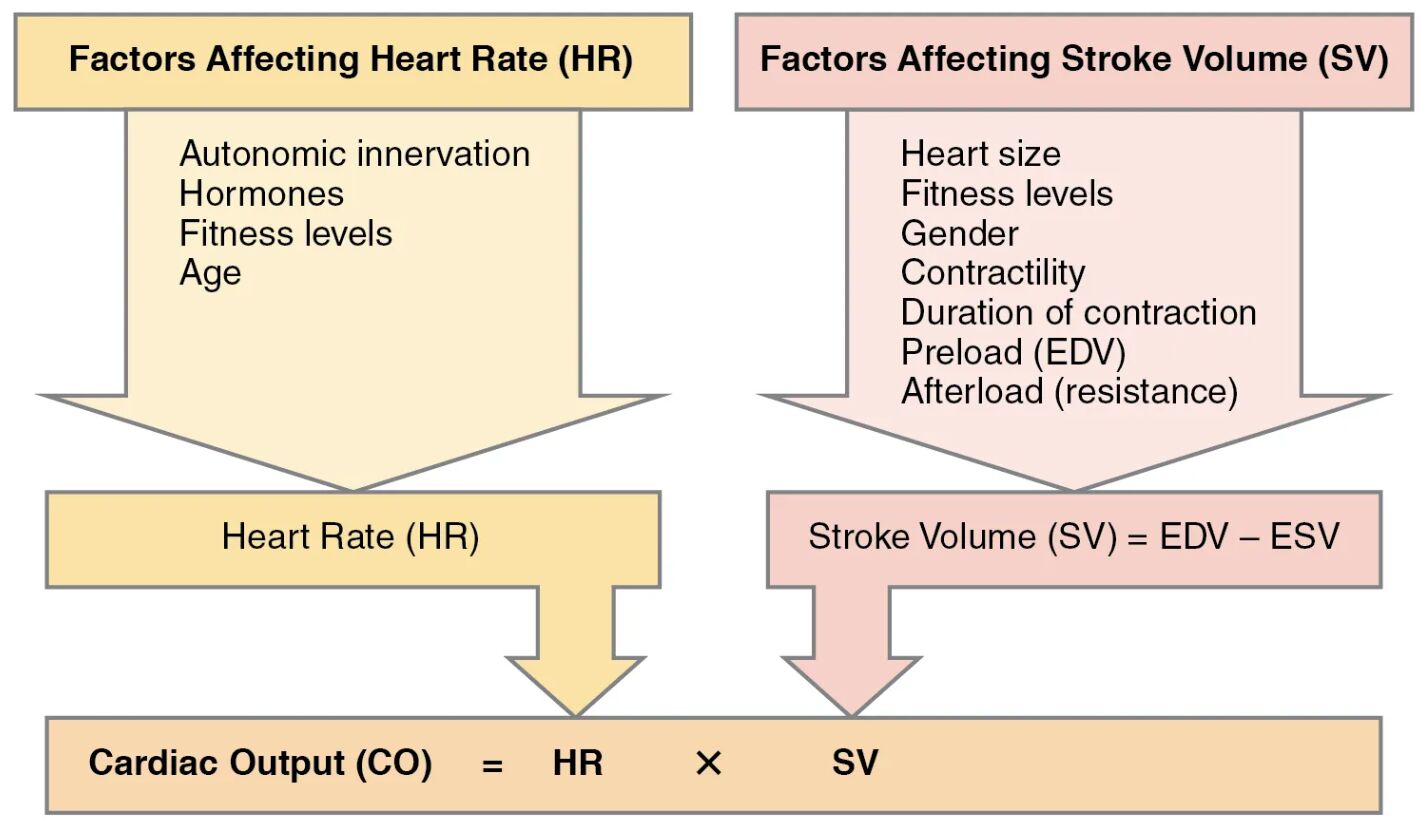
Factors Affecting Heart Rate (HR) Autonomic innervation regulates heart rate through the sympathetic and parasympathetic nervous systems, accelerating or slowing it based on bodily needs. Hormones like adrenaline and thyroxine from the thyroid gland, which releases T3 and T4, also play a significant role in modulating heart rate.
Hormones Hormones influence heart rate by altering the excitability of the sinoatrial node, with catecholamines increasing rate during stress. Thyroid hormones enhance metabolic demand, indirectly affecting cardiac pace over time.
Fitness Levels Fitness levels impact heart rate by improving cardiovascular efficiency, often resulting in a lower resting rate in well-conditioned individuals. Regular exercise strengthens the heart, allowing it to pump more blood with each beat, reducing the frequency needed.
Age Age affects heart rate as the cardiovascular system undergoes changes, with younger individuals typically having higher maximum rates. Over time, the heart’s responsiveness to autonomic signals may decline, influencing resting and exercise heart rates.
Factors Affecting Stroke Volume (SV) Heart size contributes to stroke volume, as a larger heart can hold and pump more blood per beat. This factor varies with individual anatomy and training, impacting overall cardiac performance.
Fitness Levels Fitness levels enhance stroke volume by improving the heart’s contractile strength and efficiency through regular physical activity. Trained individuals often exhibit greater stroke volumes due to enhanced myocardial adaptation.
Gender Gender influences stroke volume, with males typically having larger hearts and thus higher volumes due to differences in body size and muscle mass. Hormonal differences, such as estrogen levels, may also play a subtle role in females.
Contractility Contractility refers to the heart muscle’s force of contraction, directly affecting the amount of blood ejected. Factors like calcium ion availability and sympathetic stimulation enhance this property, boosting stroke volume.
Duration of Contraction Duration of contraction impacts stroke volume by determining how long the ventricles can eject blood. Prolonged contraction can increase output but may also signal pathological conditions if excessive.
Preload (EDV) Preload (EDV), or end-diastolic volume, is the volume of blood in the ventricles before contraction, stretching the muscle for a stronger beat. Increased venous return, as during exercise, elevates preload, enhancing stroke volume via the Frank-Starling mechanism.
Afterload (resistance) Afterload (resistance) is the pressure the heart must overcome to eject blood, influenced by arterial resistance and blood viscosity. Higher afterload, as in hypertension, can reduce stroke volume if the heart cannot compensate adequately.
Heart Rate (HR) Heart rate (HR) is the number of beats per minute, directly determining how often blood is pumped. It adjusts dynamically to meet oxygen demands, with factors like stress or fitness altering its baseline.
Stroke Volume (SV) = EDV – ESV Stroke Volume (SV) = EDV – ESV calculates the difference between end-diastolic volume and end-systolic volume, representing the blood ejected per beat. This equation highlights how filling and emptying efficiencies shape cardiac output.
Cardiac Output (CO) = HR x SV Cardiac Output (CO) = HR x SV defines the total blood flow from the heart, combining heart rate and stroke volume. This formula underscores the interdependence of these variables in maintaining circulation.
The Basics of Cardiac Output
Cardiac output serves as a cornerstone of cardiovascular function, reflecting the heart’s ability to supply blood. It adapts to physiological needs through the interplay of heart rate and stroke volume.
- Cardiac output varies with activity levels, increasing during exercise to meet oxygen demands.
- The heart adjusts heart rate via autonomic nerves, with the vagus nerve slowing it and sympathetic nerves accelerating it.
- Stroke volume depends on venous return and myocardial contractility, ensuring efficient pumping.
- Hormonal regulation, including cortisol and adrenaline, fine-tunes cardiac output during stress.
- Resting values typically range from 4 to 8 liters per minute, influenced by individual fitness.
Factors Shaping Heart Rate
Heart rate is a dynamic parameter, responding to internal and external cues. It sets the pace for blood delivery throughout the body.
- Autonomic innervation balances sympathetic (fight-or-flight) and parasympathetic (rest-and-digest) inputs.
- Hormones like epinephrine enhance heart rate by binding to beta-adrenergic receptors.
- Fitness levels lower resting heart rate through improved stroke volume efficiency.
- Aging reduces maximum heart rate, with a common estimate of 220 minus age as a peak limit.
- Emotional states, such as anxiety, can temporarily elevate heart rate.
The Role of Hormones and Innervation
Hormonal and neural influences fine-tune heart rate for optimal performance. These systems work in concert to maintain homeostasis.
- The sympathetic nervous system releases norepinephrine, increasing heart rate.
- Parasympathetic input via the vagus nerve releases acetylcholine to slow heart rate.
- Thyroid hormones T3 and T4 boost metabolic rate, indirectly raising heart rate.
- Adrenal medulla secretions during stress amplify cardiac response.
- Chronic hormonal imbalances can lead to sustained changes in heart rate.
Determinants of Stroke Volume
Stroke volume reflects the heart’s pumping efficiency per beat, influenced by multiple physiological factors. It ensures adequate blood flow with each contraction.
- Heart size determines the maximum volume the ventricles can hold.
- Improved fitness levels enhance ventricular wall thickness, boosting stroke volume.
- Gender differences affect baseline stroke volume due to anatomical variations.
- Contractility increases with calcium influx, strengthening each beat.
- Preload (EDV) rises with hydration or exercise, stretching the myocardium.
Preload and Afterload Dynamics
Preload and afterload are critical in regulating stroke volume, affecting ventricular performance. They balance filling and ejection pressures.
- Preload (EDV) increases with greater venous return, optimizing ventricular stretch.
- Afterload (resistance) rises in conditions like atherosclerosis, challenging ejection.
- The Frank-Starling law links preload (EDV) to stroke volume for self-regulation.
- High afterload (resistance) may require compensatory mechanisms like hypertrophy.
- Fluid balance directly impacts preload (EDV), influencing cardiac workload.
Clinical Implications and Monitoring
Understanding these factors aids in assessing and managing cardiovascular health. Monitoring helps detect deviations from normal function.
- Cardiac output assessment guides treatment in heart failure cases.
- Heart rate variability indicates autonomic nervous system health.
- Stroke volume monitoring via echocardiography reveals contractile issues.
- Exercise stress tests evaluate cardiac output under load.
- Medications like beta-blockers adjust heart rate and stroke volume.
In conclusion, the interplay of heart rate and stroke volume determines cardiac output, a vital indicator of heart performance. Exploring these factors deepens our understanding of cardiovascular adaptability and supports strategies for maintaining heart health. Continued research into these dynamics promises to enhance diagnostic and therapeutic approaches.

